Bilothorax (also called cholethorax or thoracobilia) is defined as the presence of bile in the pleural fluid (PF) and is a rare cause of exudative pleural effusion. Most of the cases described in the literature are associated with hepatobiliary surgery, biliary tract intervention, or biliary infections with pleurobiliary fistulas.1,2 In almost all cases, involvement was exclusively in the right pleural cavity.1
We report the case of a 58-year-old woman with a history of perihilar cholangiocarcinoma (also known as Klatskin tumor) who had undergone tumor resection surgery 10 months previously followed by chemotherapy. She was being monitored by Oncology and was, in principle, disease-free.
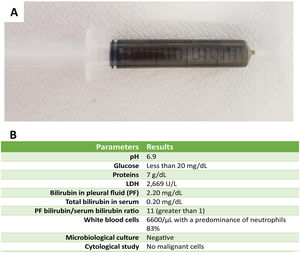
She attended the emergency department for progressive dyspnea, and a thoracoabdominal computed tomography (CT) scan revealed left pleural effusion. Post-surgical complications and bile duct fistula were ruled out. Chest ultrasound showed a moderate collection of pleural fluid, anechoic in appearance, containing fibrin tracts. Diagnostic thoracentesis was performed in the left hemithorax, and the fluid obtained was remarkable for its dark greenish and viscous macroscopic appearance, suggesting bilothorax (Fig. 1A). The PF study is described in Fig. 1B. The study was completed with diagnostic medical thoracoscopy that revealed a thickened, irregular and erythematous parietal pleura with hyperpigmented yellowish lesions. Several pleural biopsies were obtained. Pathology confirmed the suspicion of a metastatic process consistent with a relapse of perihilar cholangiocarcinoma. Finally, a tunneled chest tube was placed for better symptomatic management of the effusion.
Bilothorax is a rare cause of pleural exudate, resulting primarily from biliary tract lesions or diseases that form pleurobiliary fistulas. These include malignant or benign biliary obstruction, disruption of pleural or fissure integrity following hepatobiliary procedures (surgery or percutaneous drainage), and hepatic or subphrenic abscesses. The presence of bile in the pleural space can cause a significant inflammatory reaction and PF superinfection is common. Involvement is typically right-sided due to anatomical proximity, but bile can also pass naturally through the esophageal and aortic hiatuses, leading to involvement of the left pleural cavity.3
The most specific diagnostic criterion is a PF/serum bilirubin ratio greater than 1. Some authors propose glycolic acid in PF as an additional criterion.3
Our case is significant for left pleural unilateral involvement in the absence of recent hepatobiliary surgery or documented pleurobiliary fistula. An exhaustive review of the literature retrieved no cases of Klatskin tumor with histologically confirmed contralateral pleural metastasis manifesting as bilothorax, hence the interest of the case we describe. The treatment is the same as that of the cause: chemotherapy, in the case of our patient, or closure of fistulas if the cause is iatrogenic.
Conflict of interestsThe authors state that they have no conflict of interests.