Pulmonary rehabilitation (PR) is a comprehensive intervention based on thorough patient assessment followed by patient-tailored therapies, which include, but are not limited to, exercise training, education, and behavior change, designed to improve the physical and psychological condition of patients with chronic respiratory disease and to promote long-term adherence to health-enhancing behaviors.1 Physical exercise prescription is the cornerstone of rehabilitation in COPD patients, but performance of physical exercise is not without complications.2 Studies analyzing the complications of cardiac rehabilitation (CR) have demonstrated a low incidence of fatal and nonfatal complications. However, the incidence of complications of PR in COPD patients has not been analyzed.
The objective of this retrospective analysis with longitudinal follow-up was to identify the incidence of complications in COPD patients who performed PR in two hospitals from January 2013 to September 2016.
Patients were included if they were older than 40 years, smokers or former smokers of at least 10 pack-years, with a diagnosis of severe COPD based on a post-bronchodilator spirometry showing a FEV1/FVC <0.7 and FEV1 (% predicted) <50% and were included in the PR program. The exclusion criteria were: other respiratory diseases, cardiovascular, neurological and metabolic pathologies in the acute phase or uncontrolled.
Each training session consisted of warm-up exercises of the upper and lower limbs and the spine for 20min, followed by continuous aerobic exercise by cycling for 30min. The initial intensity of training was 50W, increasing progressively with tolerance to the exercise. This was followed by strengthening exercises of the upper limb muscles during 20min, initially without resistance, and progressively increasing with the increase in tolerance, and then 10min of stretching exercises and 10min of relaxation exercises.
The exercise intensity was controlled by the patient using the modified Borg scale (from 0 to 10). Basal oxygen flow was increased by 1l in oxygen carrier patients. The duration of a PR cycle was 12 weeks of 2 sessions per week.
Complications during PR were classified as major and minor. A major complication was defined as any event that determined the discontinuation of PR, and a minor complication allowed continuing the PR.
The ethics committee of the Hospital of Mataró (Barcelona, Spain) approved the study. The patients provided written informed consent to participate in PR, but since this was a retrospective study no specific consent was required for the analysis.
A total of 291 patients were evaluated, with 44 (15.1%) abandoning the PR program. Of these latter patients, 20 (45.4%) dropped out because of a lack of motivation, 9 (20.4%) due to difficulties in reaching the hospital, 8 (18.2%) for exacerbations and 6 (13.6%) due to concomitant diseases.
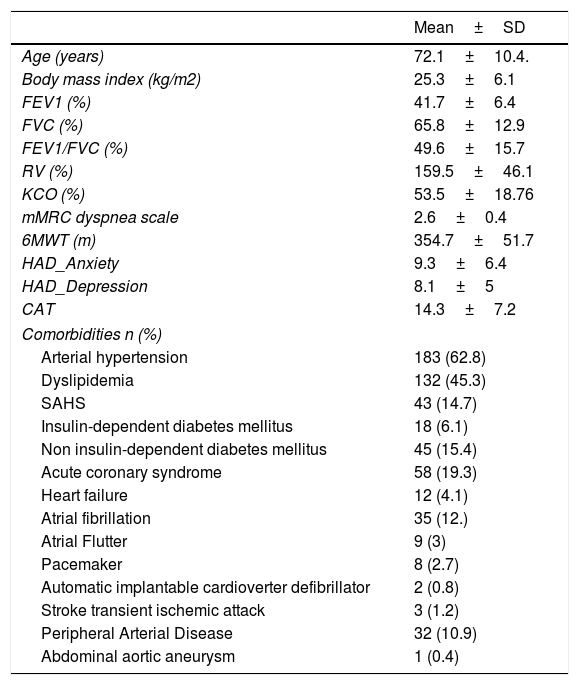
Table 1 shows the characteristics of the patients included. They underwent a mean of 17.6 (range: 2.2) PR sessions with a total of 7677h. There were 2 major complications, both in patients with previous hypertension, diabetes and dyslipemia: 1 acute coronary syndrome in a 71 years-old patient with FEV1 (%)=42% and peripheral artery disease and 1 debut of cardiac arrthymia manifested as atrial fibrillation in a 60 year-old patients with FEV1 (%)=37% and sleep apnea. Thus, the incidence of major complications was 2.7/10 000h of PR. Three minor complications were presented: 3 musculoskeletal problems involving acute low back pain and 2 increases in the sensation of dyspnea associated with O2 desaturation during physical exercise, with the incidence of minor complications being 6.5/10 000h of physical exercise.
Characteristics of the patients with COPD included in the pulmonary rehabilitation (PR) program.
| Mean±SD | |
|---|---|
| Age (years) | 72.1±10.4. |
| Body mass index (kg/m2) | 25.3±6.1 |
| FEV1 (%) | 41.7±6.4 |
| FVC (%) | 65.8±12.9 |
| FEV1/FVC (%) | 49.6±15.7 |
| RV (%) | 159.5±46.1 |
| KCO (%) | 53.5±18.76 |
| mMRC dyspnea scale | 2.6±0.4 |
| 6MWT (m) | 354.7±51.7 |
| HAD_Anxiety | 9.3±6.4 |
| HAD_Depression | 8.1±5 |
| CAT | 14.3±7.2 |
| Comorbidities n (%) | |
| Arterial hypertension | 183 (62.8) |
| Dyslipidemia | 132 (45.3) |
| SAHS | 43 (14.7) |
| Insulin-dependent diabetes mellitus | 18 (6.1) |
| Non insulin-dependent diabetes mellitus | 45 (15.4) |
| Acute coronary syndrome | 58 (19.3) |
| Heart failure | 12 (4.1) |
| Atrial fibrillation | 35 (12.) |
| Atrial Flutter | 9 (3) |
| Pacemaker | 8 (2.7) |
| Automatic implantable cardioverter defibrillator | 2 (0.8) |
| Stroke transient ischemic attack | 3 (1.2) |
| Peripheral Arterial Disease | 32 (10.9) |
| Abdominal aortic aneurysm | 1 (0.4) |
mMRC: modified Medical Research Council; 6MWT: 6-Minute walking test; RV: residual volume; KCO: carbon monoxide transfer coefficient; HADS: Hospital Anxiety and Depression Scale; CAT: COPD Assessment Test; SAHS: sleep apnea-hypopnea syndrome.
To our knowledge this is the first study to evaluate the safety of physical exercise in PR programs in patients with COPD. Although the sample size of our study was small, we observed a low incidence of complications during PR.
The most severe complications were cardiovascular and may be frequent since patients with severe COPD have usually been heavy smokers, and preexisting cardiovascular comorbidity is a normal finding and may interfere with PR programs. Our sample included patients with severe COPD with a mean age of 72 years and an elevated percentage of cardiac comorbidity, hypertension and diabetes. It is therefore important to first evaluate cardiac risk in patients with COPD who are prescribed physical exercise in a PR program by performing ergospirometry to determine the origin of limitation related to exercise, in particular in those patients at highest risk.3
The major complications observed were of cardiac origin but were not life threatening. The incidence of complications such as sudden death with exercise is very low and is almost always limited to athletes performing high intensity exercise.4 Several previous studies have evaluated the incidence of complications associated with CR. Indeed, Pavy et al. described an incidence of acute myocardial infarction in CR programs of 1.3 cases per million hours,5 while Van Camp et al. reported an incidence of 1 case per 294,118h.6 In relation to cardiac arrhythmias, an incidence of ventricular fibrillation of 1 case per 11,996h of physical exercise was observed.6 The higher rate of major complications found in our study compared with CR could be explained by the differences in the characteristics of the patients, since many low-risk patients are included in CR programs, compared to our group consisting of severe COPD with high prevalence of cardiovascular comorbidity.
With regard to the minor complications, we observed a predisposition to musculoskeletal problems. Likewise, Chen et al. demonstrated that lumbar pain is the most frequent type of musculoskeletal involvement in patients with COPD undergoing a PR program and may be presented by up to 41% of the patients.7 It is therefore important to evaluate the vertebral column in patients with COPD, the thoracic region to determine vertebral compression and the lumbar region to avoid spinal facet overload. Previous assessment allows a specific rehabilitation program of the lumbar or thoracic region to be carried out prior to initiating the PR program. Only 8 patients dropped out from the PR due to an exacerbation. Although exacerbations are usually considered adverse events in COPD studies, we did not include them as such in our analysis because they cannot be considered as secondary to exercise. Our results concur with those of Fernandez et al.8 who oberved no complications in a home-based PR program for severe COPD.
In conclusion, the results of the present study show that the prescription of physical exercise in PR programs is safe, with a low incidence of major and minor complications. Nonetheless, taking into account the higher incidence of cardiovascular disease and musculoskeletal disorders in patients with COPD, evaluations are needed prior to the prescription of a PR program in these patients in order to minimize possible complications. Larger studies are necessary to confirm our findings
AuthorshipE. Pleguezuelos, M. Miravitlles: Study design, analysis of results and drafting of the manuscript.
E. Moreno, B. Samitier, P. Ortega, X. Vila, A. Gomez, M. Majó, MV González, L. Ovejero, L. Guirao, J. Juanola: Recruitment of patients and conducting the study, participation in data analysis and revision and approval of the manuscript.