Systemic lupus erythematosus (SLE) is an autoimmune chronic systemic disease involving skin, joints and/or internal organs, such as lungs, brain and heart. SLE affects predominantly women (female to male ratio 10:1).1 Pulmonary manifestations of SLE can include a wide spectrum of diseases. The most common is lupus pleuritis. Less common is parenchymal involvement, presenting either as acute lupus pneumonitis (ALP) or chronic interstitial lung disease. Possible pulmonary manifestations of SLE are pneumonia, pulmonary embolism, pneumothorax, acute reversible hypoxemia, shrinking lung syndrome and pulmonary haemorrhage.2 It is believed that pulmonary complications are the consequence of the immune complex mediated injury.
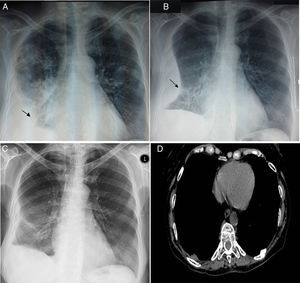
A 66-year-old woman was presented to the Emergency Department, having severe breath shortness, high temperature and chest pain. She has been suffered from systemic lupus erythematosus for 20 years, and for the last six months was using 10mg Prednisone and Methotrexate 5mg once weekly. At the examination, she was found to have elevated body temperature 38.1°C, tachycardia (120beats/min) and elevated blood pressure (160/90mm Hg). Her appearance was anorexic, diaphoretic, dyspnoeic, slightly disoriented. Her pupils were round equally with good light reaction, and her extraocular muscles were intact. She had neither neck adenopathy, nor jugular venous distention or meningismus. Precordial examination has shown no murmurs, rubs or gallops. Her breath sounds were decreased, with the right side percussion dullness. She had 2+ pitting edema to the midcalf. Examined neurologically, she had mild confusion but was nonfocal otherwise. Routine blood examination revealed normochromic normocytic anemia (haemoglobin: Hgb 11.1gm/dL), white blood cells: WBC count 24600/μL, platelets count 68000/μL and an erythrocyte sedimentation rate (ESR) 120mm in the 1st hour. Serum biochemistry revealed C-reactive protein (CRP) 3mg/dL, whereas unremarkable results were reported from urine analysis and urinoculture. Arterial blood gas analysis showed hypoxemia with respiratory alkalosis. Chest radiograph showed consolidation of the right upper lobe and a mild right-sided pleural effusion on the right side (Fig. 1A). Sputum culture, blood culture, sputum microscopy for acid fast bacilli, Mantoux test and HIV serology were negative. Treatment of the patient was started with empiric intravenous antibiotics (cefriakson, ciprofloksacin and metronidazole) accompanied with supportive care. On the 3rd day of the therapy, patient had high body temperature of 40°C and the control chest X-ray has revealed the encapsulated pleural effusion on the right side (Fig. 1B). A diagnostic thoracocentesis was performed, yielding 60mL of yellow, slightly cloudy fluid, showing a red blood cell-RBC count of 2.0×103/μL and, WBC count of 340/μL (15% leukocytes, 71% neutrophils, and 13% monocytes); pH 7.48; glucose 58mg/dL; total protein 2.46g/dL, lactate dehydrogenase 12545U/L, adenosine deaminase 51.3units/L; Ziehl-Neelsen stain negative; Gram stain and culture negative and Mycobacterium DNA polymerase chain reaction negative, with no malignant cells. Bacterial cultures were negative. Fiber-optic bronchoscopy with bronchoalveolar lavage (BAL) fluid analysis has shown epithelial cells. Since the patient had a continuously high body temperature up to 39°C and round rash emerging over the left elbow, anti-nuclear antibody (ANA) testing was performed and was positive (titer 1:1280, homogeneous pattern), with anti-ds-DNA weakly positive, while perinuclear and cytoplasmic anti-neutrophil cytoplasmic antibody (p-ANCA and c-ANCA, respectively) were negative. Serum C3 and C4 levels were decreased (30mg/dL and 7mg/dL, respectively). According to results, a diagnosis of SLE presenting with acute pneumonitis was made. On the 4th day, the patient was started with 1g intravenous methyl prednisolone once a day for 3 days, followed by tablet hydroxychloroquine 400mg daily and tablet prednisone 1mg/kg daily for 6 weeks with gradually tapering of prednisolone to a maintenance dose of 10mg daily. From two months after, her chest X-ray has shown practical resolution (Fig. 1C). At six month later, computed tomography described adhesions of the right side with no other specific abnormalities (Fig. 1D).
66-Year-old woman with systemic lupus erythematosus presenting with acute lupus pneumonitis. (A) Chest X-ray showing right pleural effusion (asterisk) and pulmonary consolidation in right upper lobe. (B) On the chest X-ray three days later, a right encapsulated pleural effusion (asterisk) was observed. (C) Practical disappearance of encapsulated effusion in the thoracic study two months later, with a thickening of the right costal pleura and a lateral costophrenic sinus. (D) Axial section of the computed tomography study at 6 months, at the level of the pulmonary bases with a mediastinum window was normal.
Acute lupus pneumonitis (ALP) is an uncommon manifestation of lupus, affecting less than 2% of cases. It is often life threatening once ventilator failure sets in, with mortality rate of more than 50%, despite of the treatment.3 The main pathology in ALP could be the acute alveolar capillary unit injury.4 Lupus pneumonitis presents with acute onset of fever, cough, tachypnea and hypoxia. The usual radiological sign of lupus pneumonitis is consolidation in one or more lung areas, typically basal and bilateral, often associated with pleural effusion and pulmonary arterial hypertension.5 Our case was difficult to diagnose at first, since the onset symptoms indicated infection etiology and do the relevant work up. We have excluded infective pneumonia by repeated sputum analyses and single BAL fluid examination; alveolar hemorrhage since there were no hemoptysias and Hemosiderin-laden macrophage was absent in BAL fluid. The mainstay of acute lupus pneumonitis treatment is the systemic corticosteroids usage (prednisone 1–1.5mg/kg/d divided accordingly), although despite high-dose corticosteroid usage, the lupus pneumonitis mortality remains high.3 If there is no response to oral corticosteroids within 72h and the patient has marked tachypnea, hypoxemia or suspected diffuse alveolar hemorrhage, treatment should include intravenous corticosteroid pulse therapy (i.e., 1g methylprednisolone per day for 3 days).3 The corticosteroid improvement was impressive in our case, noticed on the very first day.
In conclusion, acute lupus pneumonitis can be the initial manifestation of SLE. ALS diagnosis is essential, by excluding other causes of lung infiltration, such are infective pneumonia (bacterial, mycobacterial, fungal and viral), organizing pneumonia (OP), alveolar hemorrhage, pulmonary embolism and volume overload state, due to either renal failure or to congestive heart failure.6 Also, it is critically important to differentiate ALP from diffuse alveolar hemorrhage (DAH) which may have similar clinical presentation, laboratory immunology testing (ANA, anti-dsDNA) and radiographic findings, with almost equally grave prognosis. ESR and CRP may be used to support clinical suspicion. Unlike ESR, CRP (or hs-CRP) elevation is only modest in active SLE without infection, while a high hs-CRP level (>5–6mg/dL) is a strong predictor of infection. Also, ESR/CRP ratio ¿15 suggests lupus flare, while ratio ¿2 suggests infection.7