Warfarin is one of the most commonly used oral anticoagulant and is associated with several adverse reactions, including major bleeding. Thoracic hemorrhage accounts for only 3% of all hemorrhagic complications and is usually related to trauma.1 Trauma is also the major cause of pulmonary hematomas, however, there are only few reports of spontaneous pulmonary hematoma as a complication of anticoagulant therapy.2,3
We report the case of a 63-year-old man, former smoker, admitted to the emergency department with hemoptysis with onset after intense cough, secondary to a choking episode during a meal, without aspiration. He has been taking warfarin for atrial fibrillation for 15 years and, additionally, he used 100mg aspirin for 3 years, after an acute myocardial infarction. He also had chronic renal disease (stage III) and essential thrombocytosis. He vigorously denied recent episodes of trauma, including any minor trauma.
He was hypotensive (blood pressure 92/60mmHg) and oxygen saturation was 90%. On physical examination, respiratory sounds were decreased on upper half of the right hemithorax and he had irregular heartbeats sounds. Physical examination of other systems was unremarkable.
In his laboratory findings, hemoglobin was 14.2g/dl, leukocyte count 18.500/mm3, platelets 1.061.000, creatinine 1.60mg/dl (with a creatinine clearance of 47ml/min) and International Normalized Ratio (INR) level was 5.15.
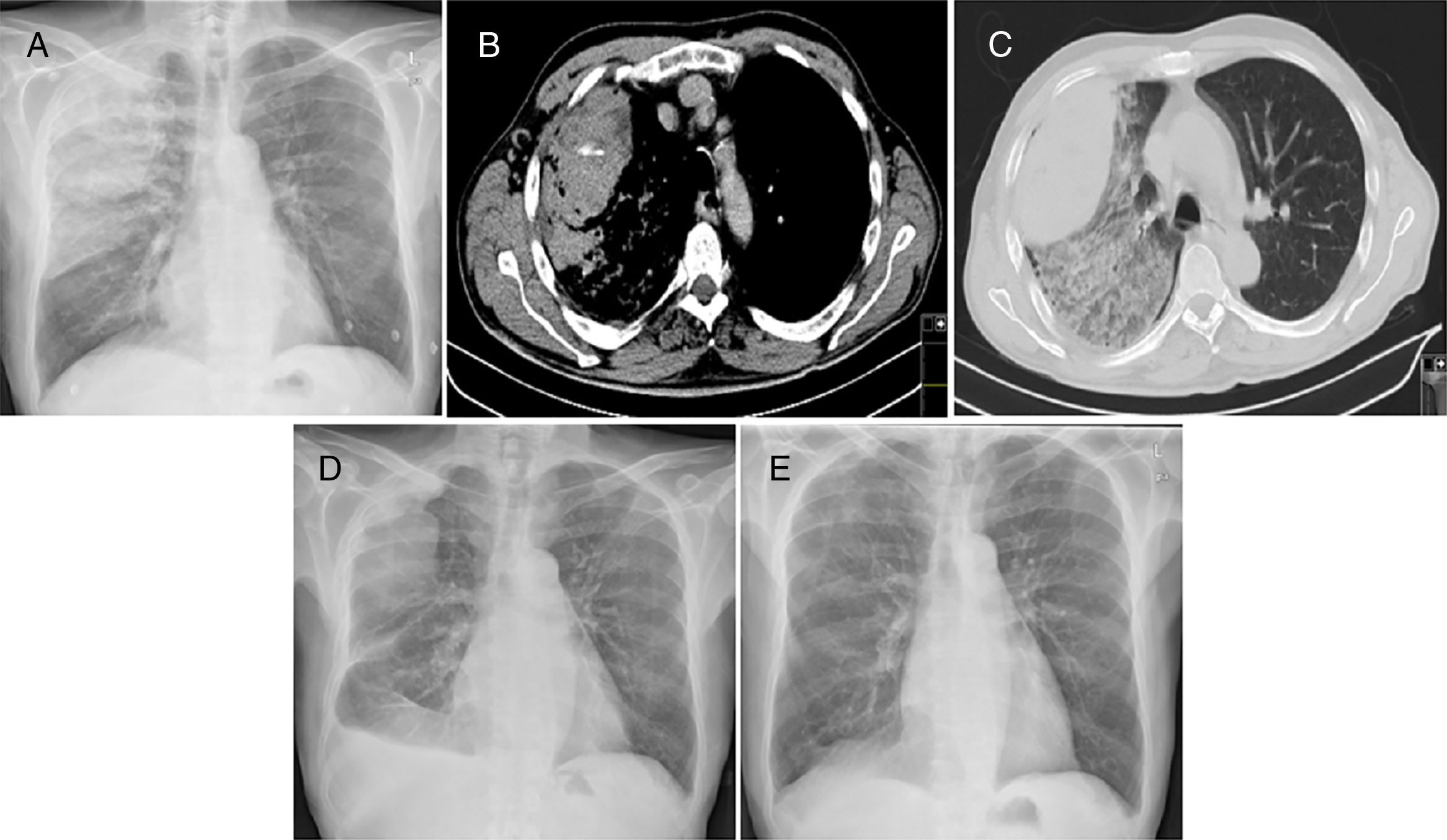
Chest X-ray revealed a heterogeneous opacity in the right upper lung field (Fig. 1A). Chest computed tomography (CT) showed a large subpleural hematoma on the right lung with 9cm in diameter and evidence of active bleeding (Fig. 1B), scattered infiltrate on the right upper lobe (Fig. 1C) and small right pleural effusion.
(A) Postero-anterior chest X-ray showing a heterogeneous opacity in the right superior lung lobe. (B) Chest CT showing a subpleural hematoma on the right lung with active bleeding. (C) Chest CT showing subpleural hematoma and scaterred infiltrate on the right upper lobe. (D) Postero-anterior chest X-ray performed at hospital discharge, showing reduction of the hematoma in the right superior lung lobe and right small volume pleural effusion. (E) Postero-anterior chest X-ray performed after 7 months, showing complete disappearance of hematoma.
The coagulation abnormality was corrected with vitamin K and 1000U of prothrombin complex concentrate and he was admitted to intensive care unit. Surgery was not performed after consultation with thoracic surgeons. He presented a gradual reduction of hemoptysis but right pleural effusion increased. A right diagnostic thoracentesis was performed and the fluid was serosanguineous, not compatible with hemothorax (pleural fluid hematocrit less than 50% of the peripheral blood hematocrit), however, given the large volume of the pleural effusion, conditioning dyspnea and respiratory failure, a chest tube was inserted during 5 days. Fiberoptic bronchoscopy was performed and excluded endobronchial lesions, bleeding or foreign body. He required transfusion of 3 units of packed red blood cells during hospitalization. The case was discussed with cardiology and, given the embolic risk associated with permanent atrial fibrillation, treatment with warfarin was restarted (with discontinuation of aspirin) and the INR maintained within the therapeutic range, without hemoptysis recurrence. The pulmonary hematoma had a progressive size reduction (Fig. 1D) and after 7 months of follow-up, chest X-ray shows complete disappearance of hematoma (Fig. 1E).
Pulmonary hematomas are collections of blood within the alveolar and interstitial spaces and usually occur by vessel rupture secondary to chest trauma. Spontaneous cases with no underlying conditions are extremely rare.4 Reported cases of spontaneous pulmonary hematoma secondary to anticoagulation therapy as heparin or warfarin and antiplatelet therapy are very small.2,3,5,6 Researchers proposed that pulmonary hemorrhage may occur in preexisting cyst or bullous emphysema via angionecrosis and erosion of the cystic wall.3,7
Our patient took warfarin for 15 years and since then he did not experience any important hemorrhagic event, even when he presented INR>7, in an internment in nephrology 4 years ago, for study of renal failure (at that time with creatinine clearance <30ml/min). Now he presented supratherapeutic anticoagulation therapy in association with aspirin that, combined with chronic renal disease and essential thrombocytosis (two diseases associated with a recognized increased risk of bleeding), probably have contributed for the massive size of the hematoma. However, it is not completely clear what triggered the formation of the pulmonary hematoma. He did not have bullous emphysema or lung cyst that could be at the origin of the hematoma. Alternatively, a minor trauma to the chest not remembered by the patient, could be the leading cause of pulmonary hematoma, although cutaneous signs of trauma were not visible. In fact, the patient started with hemoptysis after intense cough, secondary to a choking episode during a meal. We believe that the intrathoracic pressure produced by intense cough may have originated enough trauma to trigger the hematoma formation and intrabronchial bleeding, in a patient with additional risk factors for bleeding.
The treatment of our patient was mainly supportive: management in a intensive care unit, oxygen supplementation, correction of anticoagulation, transfusion of packed red blood cells and drainage of pleural effusion. Surgery was not an option for thoracic surgeons, due to high risk of uncontrollable hemorrhage by decompression of the hematoma. Due to the scarcity of described cases, the ideal treatment is not yet defined and should be individualized. Despite emerging use of the new oral anticoagulants and recognized advantages,8 it was decided, by immunohemotherapy, to maintain warfine, given the availability of antidote in case of major bleeding recurrence, in a patient with previous records of creatinine clearance <30ml/min.
In summary, although rare, spontaneous pulmonary hematoma must be kept in mind as a possible complication of anticoagulant therapy, although in our patient the additional use of antiplatelet therapy, chronic renal disease and essential thrombocytosis also had an important contribution to this complication, probably triggered by severe cough. The management of these patients can be a real challenge and the disclosure of theses rare cases may help to improve knowledge about the best therapeutic strategy.