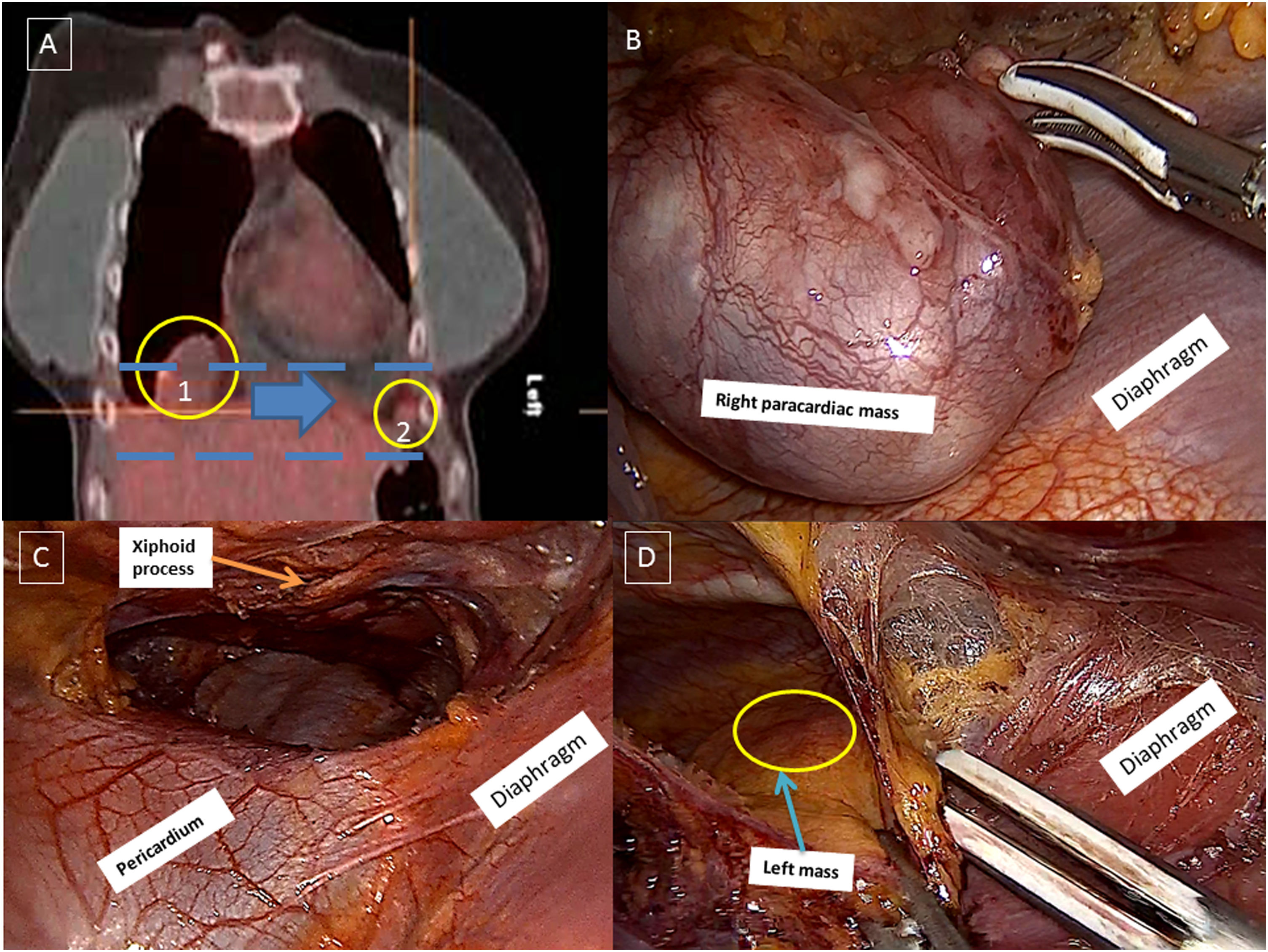
We present a case report of a 40-year-old female patient, operated for ovarian immature teratoma (grade 3) with gliomatosis peritonei. Hysterectomy with double annexectomy, appendectomy, omentectomy, lymphadenectomy (glial tissue in 1 lymph node) and the adjuvant chemotherapy was performed. One year later, recurrence disease in peritoneal form and two chest masses (right paracardiac mass: 70mm×46mm×50mm; mass in anterior left costo-phrenic angle: 7mm×15mm×5mm) on positron emission tomography follow-up was observed (Fig. 1A). The patient had ASA III and APACHE II. A combined thoraco-abdominal approach for surgical rescue was decided. To resect both thoracic tumors, we would need a bilateral thoracic approach. However, we believed that a laparotomy and bilateral videothoracoscopy in the same surgical session were very invasive approach for this patient. In addition, bilateral chest drainages and abdominal drainages could be uncomfortable. Finally, we decided a right thoracoscopic access with CO2 insufflation and medial laparotomy. Under general anesthesia with selective intubation, the patient was placed in left lateral semidecubitus position. At the start of the intervention, carbon dioxide insufflation at pressures of 5–8mmHg was used to facilitate rapid and complete lung collapse. Three right thoracoscopic ports were utilized: 5th intercostal space in anterior axillar line (5mm), 9th intercostal space in anterior axillar line (5mm) and 7th intercostal space in middle axillar line (10mm). The right paracardiac mass (Fig. 1B) and mediastinal tissue was completely resected, without any complications. Retrosternal dissection under xiphoid process (Fig. 1C) to achieve left mass (Fig. 1D) was performed. The presence of pericardium was avoided by this approach, so it is a safe and feasible procedure. After thoracic-time, radical peritonectomy, splenectomy and right hemicolectomy were performed.
(A) Positron emission tomography scan shows a right paracardiac mass (circle 1) and other mass in anterior left costo-phrenic angle (circle 2) and the retrosternal dissection pathway (blue lines and blue arrow). (B) Right paracardiac mass dissection by right videothorcoscopic approach. (C) Retrosternal pathway under xiphoid process. (D) Left mass dissection by right videothorcoscopic approach.
The chest tube was removed on the 4th day. The patient had a fever on the 5th postoperative day, and tomography scan revealed a collection in the right iliac fosse. The abdominal drainage tube placed during surgery and antibiotic treatment allowed control of this complication. Clinical and radiological progress was good, and the patient was discharged on the 13th postoperative day.
Eight months after surgery, there is no evidence of local tumor recurrence. The histological examination of specimens confirmed mature glial tissue on the surface of the peritoneum, mesentery, mediastinal tissues and pleura. The gliomatosis peritonei (GP) is the metastatic implantation of mature glial nodules in peritoneum.1,2 GP intraoperatively may be misdiagnosed as ovarian carcinomas or peritoneal tuberculosis. However, GP has a favorable prognosis.1 In rare cases, GP showed potential for malignant transformation after several years.1,2 Thus, the follow-up may be needed. In this report, we describe this innovative thoracic approach to resect bilateral lesions and the extremely rare presence of glial tissue outside abdominal cavity and in lymph nodes in the setting of ovarian immature teratoma.
Conflict of InterestsThe authors state that they have no conflict of interests.