Residential radon is considered the second cause of lung cancer and the first in never smokers. Nevertheless, there is little information regarding the association between elevated radon levels and small cell lung cancer (SCLC). We aimed to assess the effect of residential radon exposure on the risk of SCLC in general population through a multicentric case–control study.
MethodsA multicentric hospital-based case–control study was designed including 9 hospitals from Spain and Portugal, mostly including radon-prone areas. Indoor radon was measured using Solid State Nuclear Track Detectors at the Galician Radon Laboratory.
ResultsA total of 375 cases and 902 controls were included, with 24.5% of cases being women. The median number of years living in the measured dwelling was higher than 25 years for both cases and controls. There was a statistically significant association for those exposed to concentrations higher than the EPA action level of 148Bq/m3, with an Odds Ratio of 2.08 (95%CI: 1.03–4.39) compared to those exposed to concentrations lower than 50Bq/m3. When using a dose-response model with 100Bq/m3 as a reference, it can be observed a linear effect for small cell lung cancer risk. Smokers exposed to higher radon concentrations pose a much higher risk of SCLC compared to smokers exposed to lower indoor radon concentrations.
ConclusionsRadon exposure seems to increase the risk of small cell lung cancer with a linear dose-response pattern. Tobacco consumption may also produce an important effect modification for radon exposure.
Lung cancer is the first cause of cancer death in developed countries.1 According to GLOBOCAN 2018, the annual number of new cases in the world is 2.093.876 in both sexes, with 1.761.007 deaths. In Europe, it represents 26.3% of all cancer deaths.2 5-Year survival ranges between 15% and 20% in developed countries.3 Lung cancer histological subtypes are classified in non-small cell cancer (NSCLC) and small cell lung cancer (SCLC) based on neoplastic cell characteristics. Small cell lung cancer comprises around 14% of lung cancer cases.4 Each subtype shows a different behaviour, evolution, treatment and prognosis, with SCLC having the worst prognosis of all lung cancers.
In the last years, the incidence of SCLC has been decreasing, but there is an increasing incidence in women. The historical male/female ratio was 3:1 and nowadays is 1:1. This change in the male/female ratio has been attributed to a higher frequency of tobacco consumption in women. The main risk factor of lung cancer is tobacco consumption, and SCLC is the lung cancer type most associated with this habit.5 Nevertheless, few information is available on other risk factors, such as residential radon, due to its relatively low frequency compared to other histological types.
Radon is a noble gas produced as a consequence of the decay of the Uranium found in the soil and rocks of the earth crust. Its presence is heterogeneous worldwide, depending mostly on the Uranium content of the bedrocks where buildings are present. As recognized by WHO and the US Environmental Protection Agency,6 after tobacco, residential radon is the second most important risk factor for lung cancer, and the first in never smokers. Radon decay emits alpha particles which may cause damage in the cell lining of the lung. Some studies have shown an association between radon exposure and p53, ALK or EGFR (epidermal growth factor receptor) alterations7,8 but there are no specifical studies analyzing the influence of radon in small cell lung cancer. The available evidence highlights that indoor radon might have an important role on SCLC onset. The pooling study by Darby et al. showed that, for SCLC, indoor radon increased the risk of lung cancer by a 31.2% per 100Bq/m3 vs 2.6% compared to other subtypes,9 and other research by Barros-Dios et al. showed that SCLC was the histological type most associated with indoor radon.10
The objective of the Small Cell Study was to determine the association between residential radon and small cell lung cancer and to test the possible interaction or effect modification between radon exposure and tobacco consumption. To do this we recruited exclusively small cell lung cancer cases in a multicentric case–control study performed in a radon prone area.
Materials and MethodsDesign and SettingThe Small Cell study is a hospital-based multicentric case–control study, involving 9 Spanish hospitals from 4 regions and a Portuguese hospital: Hospital Clínico Universitario de Santiago de Compostela, Hospital Álvaro Cunqueiro de Vigo, University Hospital Complex of Ourense, University Hospital Complex of A Coruña, University Hospital Lucus Augusti, Central University Hospital of Asturias, Ávila Healthcare Complex, Puerta de Hierro University Hospital and Centro Hospitalar do Porto. The study details and preliminary results have been published elsewhere.11 Incident cases with pathological diagnosis of SCLC were prospectively recruited. Controls consisted in patients undergoing non-complex surgery unrelated to tobacco consumption (i.e. inguinal haernias, major ambulatory surgery). There was no upper age limit for inclusion. Both cases and controls were older than 30 years and without neoplastic antecedents. Controls were frequency matched with cases through gender and age distribution to ensure comparison on both characteristics. The study protocol was approved by the CEIC of the Health Area of Santiago de Compostela with the reference 2015/222. To carry out the research, the STROBE guidelines for the communication of results of observational studies have been followed.12
Recruitment and Data CollectionResearchers from each participating centre recruited all SCLC cases who met eligibility criteria, and conducted a personal interview using a questionnaire focused on lifestyle factors and tobacco consumption. This questionnaire has been previously used in other investigations to analyze tobacco consumption. Details of the survey can be found elsewhere.10,13 Controls were also recruited in the participating hospitals.
Determination of Residential RadonAll study participants were given a radon detector along with placement instructions. This detector was an alpha-track device which was placed for a period of at least three months in each dwelling. Afterwards, the detectors were sent back to the Galician Radon Laboratory where results were obtained. All participants were informed on their respective indoor radon concentrations. This Laboratory is one of the three facilities accredited by the Spanish National Accreditation Entity to measure indoor radon according to the International Standards (ISO/IEC 17025:2017).
Statistical AnalysisAn univariate and bivariate descriptive analysis was conducted to determine the distribution of the study variables. A multivariate logistic regression was performed afterwards, where the dependent variable was the case or control status and the independent variable were residential radon levels, broken down into 4 categories (<50, 50–100; 101–147 and >147Bq/m3). As adjustment variables we included age (continuous), gender, education and tobacco consumption divided in never-smokers, light smokers (1–33 pack-years), moderate smokers (34–66 pack-years) and heavy smokers (>66 pack-years). Results are expressed as Odds Ratios with their 95% confidence intervals.
We tested the additive or multiplicative interaction between tobacco consumption and residential radon exposure creating a variable with 4 categories classifying individuals as exposed or nonexposed to radon, and classifying tobacco consumption in 4 categories, from heavy smokers to never-smokers. The confidence intervals of the multiplicative model were calculated using the method proposed by Figueiras et al.14 The synergy index and the confidence intervals of the multiplicative model were calculated using the method proposed by Hosmer and Lemeshow.15 Generalized additive models (GAM) were also performed to analyze residential radon (continuous) using the same covariates as in the previous analysis. This analysis was performed using R statistical software (version 3.3.0). All these analyses were performed with IBM SPSS v22 (IBM, Armonk, NY, USA).
ResultsA total of 375 cases and 902 controls were recruited. 24.5% of cases were women. The median age at diagnosis was 66 for cases compared to 61 for controls. 6.4% of the cases were younger than 50 years. Tobacco consumption was higher for cases compared to controls. Residential radon concentrations were higher than 147Bq/m3 in 161 SCLC cases (42.9%) vs 366 controls (40.6%). Median residential radon concentration was also higher in SCLC cases compared to controls (152.5Bq/m3 vs 142Bq/m3). The median number of years living in the measured dwelling was higher than 25 years for both cases and controls. A detailed description of the characteristics of cases and controls is presented in Table 1.
Description of Included Cases and Controls.
| Variable | Cases n (%) | Controls n (%) |
|---|---|---|
| Participants included | 375 (29.4) | 902 (70.6) |
| Age (years) | ||
| ≤50 | 24 (6.4) | 182 (20.2) |
| 50–70 | 234 (62.4) | 555 (61.5) |
| >70 | 112 (29.9) | 163 (18.1) |
| Median age (25–75th percentiles) | 66 (59–72) | 61 (53–68) |
| Gender | ||
| Female | 92 (24.5) | 298 (33.0) |
| Male | 283 (75.5) | 604 (67.0) |
| Education | ||
| No formal studies | 49 (13.1) | 27 (3.0) |
| Primary school | 212 (56.5) | 488 (54.1) |
| High school | 73 (19.5) | 229 (25.4) |
| University degree | 27 (7.2) | 147 (16.3) |
| Tobacco consumption | ||
| Never-smokers | 29 (7.7) | 376 (41.7) |
| Light smokers | 58 (15.5) | 290 (32.2) |
| Moderate smokers | 132 (35.2) | 136 (15.1) |
| Heavy smokers | 85 (22.7) | 54 (6.0) |
| Residential radon exposure Bq/m3 | ||
| <50 | 19 (5.1) | 64 (7.1) |
| 50–100 | 71 (18.9) | 172 (19.1) |
| 101–147 | 61 (16.3) | 151 (16.7) |
| ≥147 | 161 (42.9) | 366 (40.6) |
| Median radon concentration (25–75th percentiles) | 152.5 (91–260) | 142 (89–267) |
| Years (median) living in the measured dwelling (25–75th percentiles) | 29 (15–40) | 26 (14–38) |
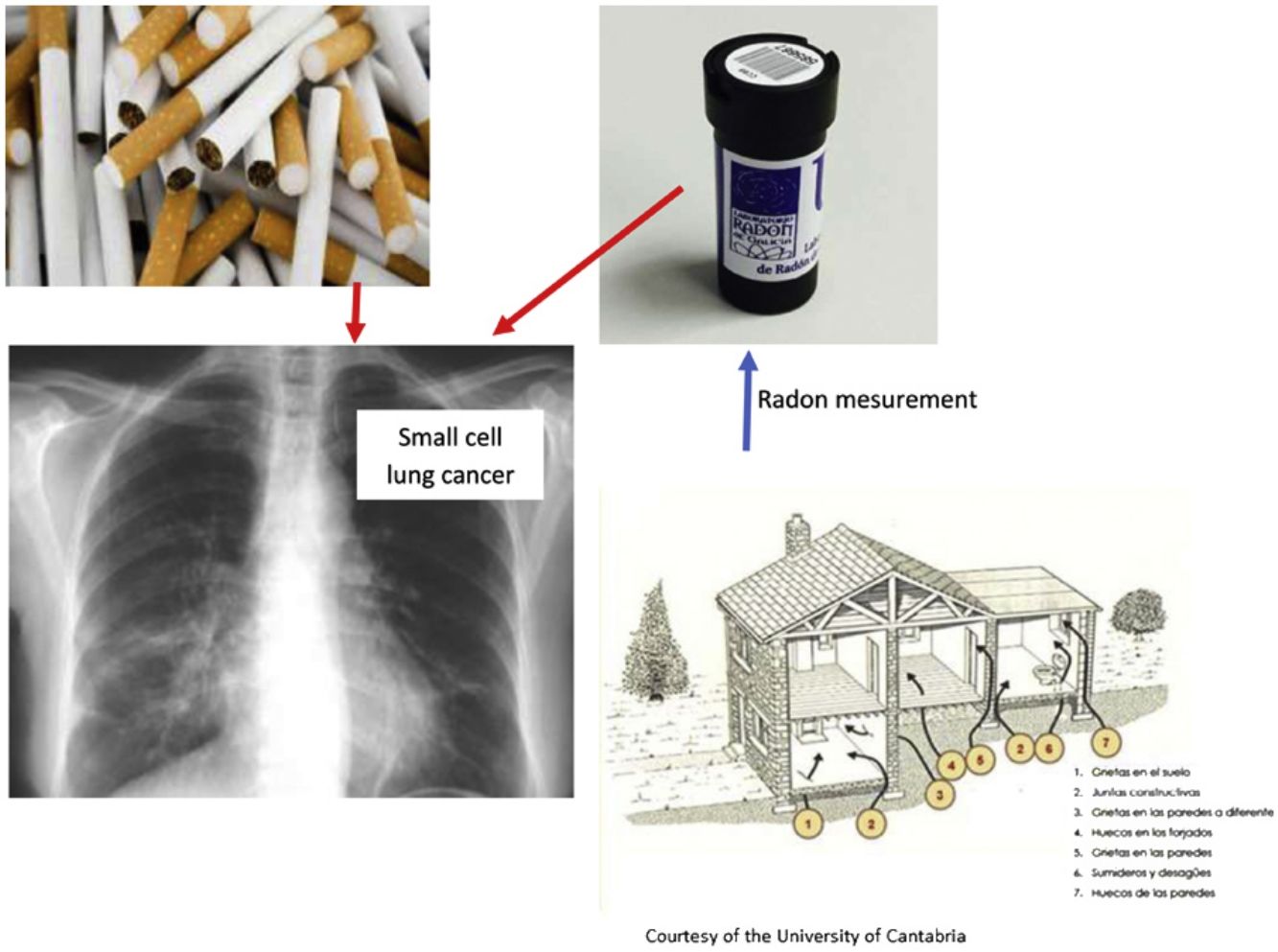
Table 2 shows the relationship between indoor radon and small cell lung cancer risk. There is a significant statistical association for those exposed to concentrations higher than the EPA action level of 148Bq/m3, with an Odds Ratio of 2.08 (95%CI: 1.03–4.39) compared to those exposed to concentrations lower than 50Bq/m3. Fig. 1 shows a GAM model that uses 100Bq/m3 as a reference level, where there seems to be a linear association between radon levels and SCLC risk.
Residential Radon Exposure and Small Cell Lung Cancer Risk.
| Variable | Cases, n (%)d | Controls, n (%)d | ORa (95%CI) | ORb (95%CI) | ORc (95%CI) |
|---|---|---|---|---|---|
| Residential radon exposure Bq/m3 | |||||
| <50 | 14 (5.7) | 63 (8.9) | 1 (–) | 1 (–) | 1 (–) |
| 50–100 | 56 (23.0) | 163 (22.9) | 1.68 (0.93–3.16) | 1.97 (1.06–3.81) | 1.59 (0.75–3.50) |
| 101–147 | 47 (19.3) | 146 (20.5) | 1.79 (0.98–3.39) | 2.30 (1.23–4.51) | 1.66 (0.77–3.71) |
| ≥147 | 127 (52.0) | 339 (47.7) | 1.91 (1.10–3.47) | 2.18 (1.22–4.10) | 2.08 (1.03–4.39) |
| Tobacco consumption | |||||
| Never-smokers | 26 (10.7) | 321 (45.1) | 1 (–) | ||
| Light smokers | 45 (18.4) | 240 (33.8) | 6.06 (3.24–11.83) | ||
| Moderate smokers | 100 (41.0) | 105 (14.8) | 28.45 (15.28–56.02) | ||
| Heavy smokers | 73 (29.9) | 45 (6.3) | 43.93 (22.10–92.00) | ||
The figures correspond to the data used in the model adjusted for all covariates. The number of participants included in different radon categories presents slight differences with Table 1 because some participants lack information on some of the adjustment variables, mainly that used to calculate pack-years. They were excluded from the analysis.
To analyze the relationship between indoor radon exposure combined with tobacco consumption we created categories combining both exposures and showing the odds ratios for different combinations (Table 3). It can be observed that for people exposed to more than 147Bq/m3 the risk of lung cancer increased with tobacco consumption. For heavy smokers, the risk of lung cancer also increases with radon exposure. Those exposed to more than 147Bq/m3 and heavy smokers showed an OR of 72.6 (95%CI 18.0–499.4) compared to never-smokers exposed to less than 50Bq/m3. The synergy index, calculated for 2 categories of radon exposure (<100 and >147Bq/m3) and tobacco consumption (never smokers and heavy smokers) was not significant: 2.18 (95%CI: 0.88–5.43).
Effect Modification Between Residential Radon Exposure and Tobacco Consumption on the Risk of Small Cell Lung Cancer.
| Tobacco Consumption (Cases, Controls); ORa (95% CI) | ||||
|---|---|---|---|---|
| Residential Radon Exposureb | Never-smokers | Light Smokers | Moderate Smokers | Heavy Smokers |
| <50 | 2, 33 | 3, 16 | 7, 8 | 3, 6 |
| 1 (–) | 5.59 (0.82–47.25) | 19.97 (3.75–159.26) | 15.00 (1.94–142.71) | |
| 50–100 | 3, 73 | 7, 57 | 28, 21 | 20, 14 |
| 0.68 (0.11–5.48) | 3.88 (0.84–27.80) | 39.87 (9.97–271.61) | 40.48 (9.50–286.07) | |
| 101–147 | 2, 58 | 12, 57 | 20, 24 | 13, 10 |
| 0.53 (0.06–4.73) | 6.74 (1.63–46.21) | 25.79 (6.34–176.92) | 35.21 (7.62–260.80) | |
| ≥147 | 19, 160 | 25, 115 | 50, 54 | 39, 15 |
| 2.09 (0.55–13.74) | 6.67 (1.77–43.81) | 28.03 (7.55–183.56) | 72.61 (17.95–499.41) | |
The number of participants included in different radon categories presents slight differences with Table 1 because some participants lack information on some of the adjustment variables, mainly that used to calculate pack-years. They were excluded from the analysis.
To our knowledge, the Small Cell study is the first multicentric case–control study focused exclusively on analysing Small Cell Lung Cancer and its risk factors, with special emphasis on its potential association with residential radon exposure. This study suggests an association between higher concentrations of residential radon concentration (>148Bq/m3 according to the United States Environmental Protection Agency16) and SCLC risk. It is evident a risk modification when indoor exposure is combined with tobacco consumption, though the interaction term for a multiplicative model did not reach statistical significance. For those with a similar tobacco habit, the increase in radon exposure seems to increase importantly the risk of lung cancer. It is important to highlight the high sample size of the present study compared to other studies performed before.17
The linear association observed between radon and lung cancer risk was also observed in other previous studies such as the one by Darby et al.9; Blot et al.19; Pershagen et al.18; Svensson et al.19; Saccomanno et al.20 and Barros-Dios et al.10 These studies support the findings of the present study which were detailed in a systematic review.18
There was no statistical synergism between radon exposure and tobacco consumption. Nevertheless, though not significant in mathematical terms, there seems to be an effect modification between both risk factors. It should be taken into account that the current study is limited by the fact that the reference category includes a low number of participants because cases of SCLC in never smokers are extremely infrequent. In our previous studies,10 a submultiplicative interaction between radon exposure and tobacco consumption was found. These results are in agreement with other previous case–control studies,10,20 concluding that there is an additive or submultiplicative effect with elevated residential radon levels in smokers compared to never smokers. Darby et al.9 also observed a greater absolute risk of SCLC in smokers versus never smokers. Barros-Dios et al.11 describes a submultiplicative interaction between radon exposure and tobacco consumption. Other studies, such as the Iowa Radon Lung Cancer Study did not show differences in the effect of residential radon for different smoking categories.21 Therefore, though the synergy index has not been significant, it can be observed that the effect was close to significance. This is also supported by a simple data observation in Table 3, where the risk of lung cancer increases importantly with the combination of both exposures, suggesting a submultiplicative interaction.
The biological mechanisms by which radon decay products cause lung cancer are not well known. They could possibly induce genetic and epigenetic changes in the neoplastic process, as some studies point out.22 Polonium 218 and Polonium 214 emit alpha particles which can induce mutations in the DNA, chromosomic aberrations, and finally a deregulation of the cell cycle.23,24 Many molecular pathways are being investigated, and the role of multiple genes such as p53, NOTCH, EGFR, ALK, NK2homeobox1, PTEN, HIF1, CHD7 is being studied.25 There is currently no biological mechanism which might explain why SCLC could be the histological type most associated with radon exposure. A possible explanation would be the fact that since SCLC is the histological type most associated with tobacco consumption, and given the submultiplicative effect observed between radon and tobacco, this possible higher risk for SCLC could be due to the interaction of both risk factors. We can hypothesize that the central location of this type of tumour affecting large bronchi could be related with radon exposure. Solid short-life descendants of radon could be deposited there more easily, or these large bronchi might receive a higher radiation dose than distal alveoli. The potential synergy between tobacco and radon exposure is also biologically plausible. Some experimental studies have shown that tobacco and radon could interact, raising the risk of lung cancer.26
This study has some limitations. Although the sample size is higher than other similar individual studies, an even more larger sample size would be required to obtain more accurate results and to test the interaction between radon and tobacco. This is also necessary to better analyze the effect of tobacco through different categories of radon exposure. Though the median age at diagnosis was a bit higher in cases than controls, we think that this fact has not influenced the results because most participants lived for more than 25 years in the same dwelling, allowing a for a long induction period for radon to cause lung cancer for both cases and controls.
This study has also some important strengths. It has been carried out in radon prone areas of Spain and Portugal, facilitating the obtention of dose-response patterns due to the high variability of radon exposure. This investigation is also multicentric, increasing external validity and reducing the possibility of a selection bias. The fact that all lung cancer cases are diagnosed in the participating hospitals covering different catchment areas guarantees a better representativeness. In addition, the return rate of the radon detectors was very high, higher than 85% for both cases and controls.
To conclude, radon exposure seems to increase the risk of small cell lung cancer, with a significant lung cancer risk departing from 148Bq/m3, and there is also a linear dose-response pattern. Tobacco consumption may produce an important effect modification for radon exposure. Those individuals exposed to high radon concentrations and heavy smokers can have a very high risk of this cancer type compared with their low exposed and never-smoking counterparts. It is necessary to increase radon awareness among citizens and administrations in order they can promote the necessary protective and mitigation measures against residential radon.
FundingPI15/01211 – ISCIII – co-financed FEDER.
This article is part of Angeles Rodriguez-Martínez doctoral thesis.
Conflicts of InterestThe authors declare not to have any conflict of interest.