Adenoid cystic carcinoma is a malignancy primarily originating from the minor salivary and submandibular glands, with rare instances of development in secretory glands of other tissues, such as the trachea.1 Primary Tracheal Adenoid Cystic Carcinoma (TACC) represents approximately 1.2% of upper respiratory tract neoplasms.2 We subsequently present a case of inoperable primary TACC.
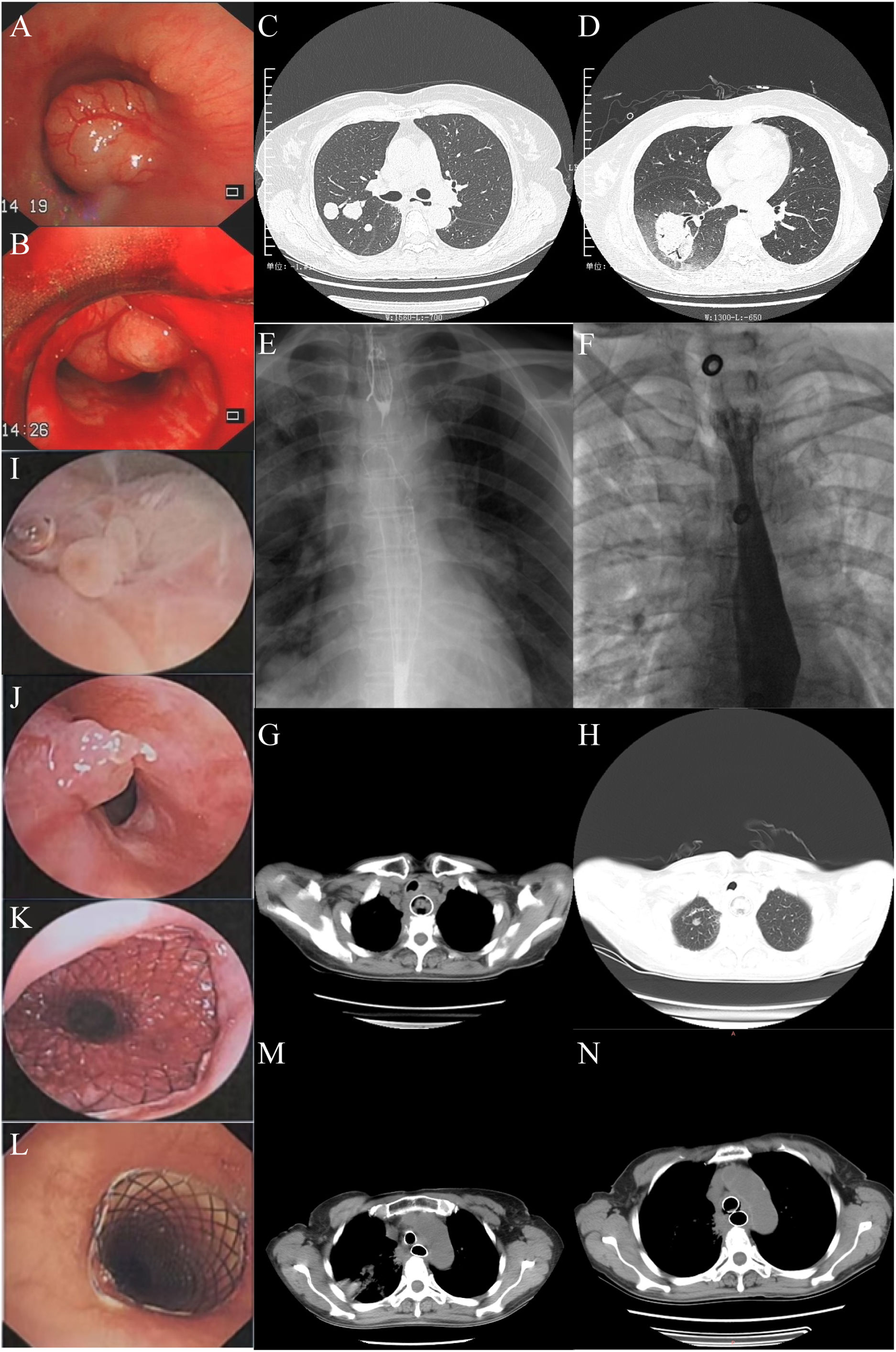
A 60-year-old female, with no active smoking history or familial cancer history, presented with a two-year history of dyspnea and concurrent osteoarthritis. In March 2015, bronchoscopy revealed a pedunculated tumor in the inferior third of the trachea, occluding roughly 90% of the airway. The pathologic diagnosis confirmed TACC. Due to carina invasion (Fig. 1A, B) and elevated surgical risk, bronchoscopic tumor reduction was pursued, followed by postoperative radiotherapy following a 70Gy/35f/2Gy regimen. In September 2019, a chest CT scan revealed multiple nodules in the right lung, suggestive of metastasis. The patient underwent a year of combined treatment with apatinib and vinorelbine. In August 2020, a new nodule emerged in the left lung, while the right lung nodule increased in size. Percutaneous lung puncture pathology confirmed TACC (right). The patient underwent argon-helium cryoablation therapy (right) (Fig. 1C, D) in October. In July 2021, the bilateral lung nodules grew, and the patient could not undergo further ablation treatment. Since September 2021, the patient underwent multiple tracheal tumor resections and local injections (endostar+cisplatin) due to the recurrence of endotracheal lesions. In December 2022, the patient experienced dysphagia, with upper gastrointestinal angiography revealing stenosis. An esophageal stent was subsequently inserted under digital subtraction angiography (DSA) guidance (Fig. 1E, F), however, the patient developed mild dyspnea due to tracheal compression. In June 2023, the patient presented with recurrent difficulty in breathing and swallowing. A chest CT scan revealed near-total occlusion of the upper gastrointestinal tract lumen and new tracheal neoplasms (Fig. 1G, H). The patient underwent bronchoscopy, and the neoplasms in the esophagus and trachea were excised. Pathology revealed granuloma (esophagus), and the esophageal stent was repositioned to cover the neoplasia (Fig. 1I–K). Later, tracheoscopy revealed an airway stenosis of approximately 80%, and a Y-shaped metal-covered stent was inserted (Fig. 1L), with efficacy evaluated by chest CT scan (Fig. 1M). A month later, a digestive-respiratory tract fistula developed (Fig. 1N), and the patient is currently undergoing anti-infective treatment.
(A and B) A huge pedunculated round mass in the inferior third of the trachea (20/3/2015). (C and D) Right lung tumor before and after receiving argon-helium cryoablation targeted therapy (30/10/2020; 4/11/2020). (E and F) Esophageal stenosis, and then esophageal covered metal mesh stent (MTN-SE-S-20/100-A-8/650) implantation under DSA (5/1/2021; 6/1/2021). (G and H) Tracheal space occupying, esophageal space occupying after esophageal covered metal mesh stent implantation (7/6/2023). (I and J) Rigid bronchoscopy combined with flexible bronchoscopy to remove the new organisms in the esophagus and then move the esophageal covered metal mesh stent up 1cm(7/6/2023). (K and L) Rigid bronchoscopy combined with flexible bronchoscopy to remove tracheal new organisms and then Y-shaped covered metal mesh stent (size: 16mm×50mm trachea/12mm×35mm left principal bronchus/15mm×35mm right principal bronchus) was implanted (7/6/2023; 9/6/2023). (M) Chest CT was used to evaluate the placement of double stents (10/6/2023). (N) Digestive-respiratory tract fistulas (8/7/2023).
In comparison to fully resected TACC, patients with inoperable TACC exhibit reduced survival rates (10-year survival rate 63.4% vs. 46.4%), with the optimal treatment strategy remaining elusive.3 Radiotherapy can mitigate the risk of local TACC recurrence, although it shows limited sensitivity to chemotherapy. Vascular-targeting drugs can decelerate its growth rate, but the lack of clinical studies hampers accurate efficacy evaluation.4 We consider our case to be of significant relevance. Firstly, choosing treatment for inoperable TACC is an immense challenge. We documented the comprehensive treatment journey of a TACC patient with prolonged survival, consistently adhering to the principles of palliative care. Secondly, this case serves as a reminder that for advanced TACC patients requiring dual tracheal and esophageal stents, vigilance toward the development of tracheo-esophageal fistula is crucial.5
Authors’ contributionsJun Teng: Conceived and design of the study, drafting the article, and approval of the final version.
Heng Zou: Acquisition of data, critical revision and approved the manuscript.
Hongwu Wang: Design of the study, agreement to be accountable for all aspects of the manuscript in ensuring that questions related to the accuracy or integrity of any part of the manuscript are appropriately investigated and resolved, read and approved.
Institutional review board statementThe Ethics Committee of Dongzhimen Hospital Affiliated with the Beijing University of Chinese Medicine (Project ID: 2023DZMEC-450-01).
Informed consent statementParticipant was fully informed of the study and gave their informed written consent before participation. This study was conducted in accordance with the Declaration of Helsinki.
Data availability statementThe data that support the findings of this study are available from the corresponding author upon reasonable request.
Consent for publicationAll authors agree to the publication of this article.
FundingThis research was funded by the innovative development project for young physicians of the professional committee of respiratory disease drug research of china association of traditional Chinese medicine (No. HXQNJJ-2023-014).
Conflicts of interestThe authors declare no conflict of interest.
We also thank OpenAI for granting us access to their language model, ChatGPT, which assisted us in improving the language quality of this paper.