Nuclear protein in testis (NUT) carcinomas (NC) are rare, highly aggressive tumors.1–3 Their genetic characterization involves a chromosomal rearrangement of the NUTM1 (NUclear protein in Testis Midline carcinoma family member 1) gene in chromosome 15q14, typically alongside a gene from the bromodomain-containing protein (BRD) family, commonly BRD4 (75% of the cases).1–3 NC is underdiagnosed, likely due to nonspecific histological presentation and lack of physician awareness.1 Pulmonary NC typically presents in non-smokers under 40 years-old with no gender preference and unspecific symptoms, such as cough, dyspnea, chest pain or hemoptysis.2,4 Large unilateral lung masses are common, occasionally accompanied by pleural effusion or atelectasis. Distant metastasis are present in 96% of pulmonary NUT carcinomas.2 Histologically, it overlaps with other poorly differentiated neoplasms.1,3 Diagnosis is confirmed by immunohistochemistry, with NUT monoclonal antibodies or molecular genetic testing.1–3 In a recent review including 40 cases of NC, the mean overall survival (OS) for primary pulmonary NC was 6.21 months.4 Surgery is associated with improved OS and PFS,2,4,5 although the inaccessibility of some tumors and advanced stages limits this approach.2–4 Concurrent or sequential chemoradiotherapy, sometimes in combination with immunotherapy,2 seems to prolong OS.4 Newer treatments are under research, including histone deacetylase inhibitors and bromodomain and extraterminal (BET) inhibitors.2–4
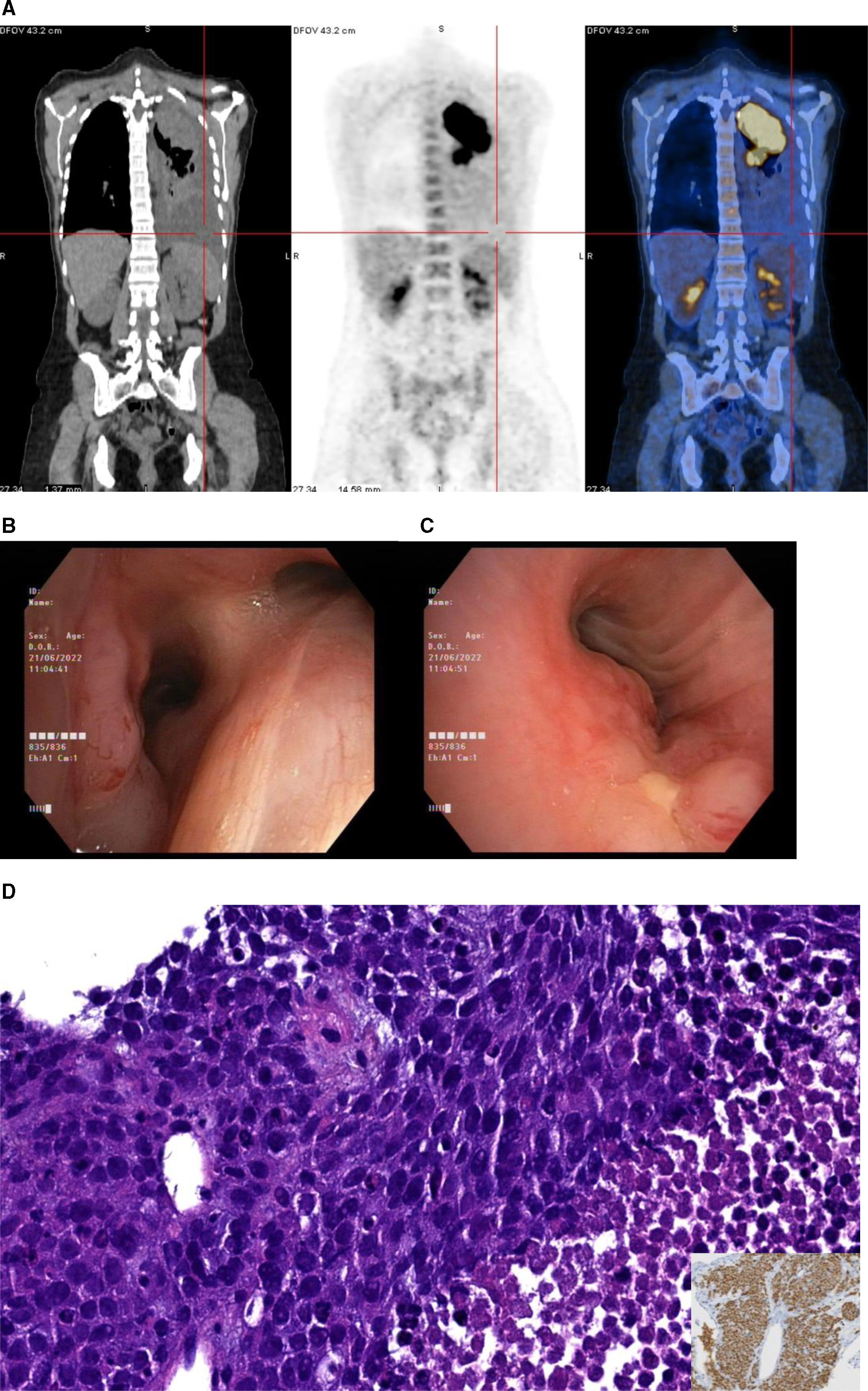
A 43-year-old female, non-smoker, with no relevant comorbidities, presented with pleuritic chest pain and exertional dyspnea lasting 1 month. Chest CT-scan revealed an invasive mediastinal mass (11.3cm craniocaudal diameter), and left pleural effusion. PET-CT scan (Fig. 1A) showed contrast uptake in a left upper lobe mass (Standardized Uptake Value (SUV) 25.4), mediastinal, supraclavicular and cervical adenopathies, left pleural effusion, and a lesion in the left iliac bone. Videobronchoscopy showed total occlusion of left main bronchus (Fig. 1B, C). Bronchial biopsy samples revealed an undifferentiated malignant epithelial neoplasm with small, round, blue cells. Imunohistochemistry was positive for vimentin and a dot-like positivity in some cells for CK8/18, while CK7, CD56, chromogranin, synaptophysin, p40, TTF-1, CD3, CD20, CD45, S100 protein, CD99, WT1, MSA, SMA, desmin, MyoD1 and TLE1 were negative; Ki67 was 90%. A pathology diagnosis of undifferentiated neoplasm was made and a stage IV-A thoracic small-cell lung cancer without neuroendocrine differentiation was assumed. Palliative chemotherapy with carboplatin and etoposide was initiated. After 3 cycles, disease progression occurred, with pericardial effusion. Second-line chemotherapy with topotecan was initiated. Due to lack of response to chemotherapy, the initial diagnosis was questioned. A transthoracic lung biopsy was ordered; results pointed to undifferentiated small-cell sarcoma with round blue cells (Fig. 1D). NGS showed a BRD4(11)-NUTM1(12) fusion. Immunohistochemistry for NUT expression showed intense nuclear expression in malignant cells. The patient died a few days later, 7 months after the initial diagnosis, before additional therapy was initiated.
(A) PET-CT scan depicting a large mass in the left upper lobe with extension to the mediastinal region and to the ipsilateral broncho-hilar region, as well as left pleural effusion. (B, C) Videobronchofibroscopy images: (B) Vegetant mass in the anterior traqueal wall, (C) Complete obstruction of left main broncus, (D) Pathological samples: H&E, ×40: Histological examination showed a highly cellular solid neoplasm, with sheets and nests of small to intermediate-sized undifferentiated cells with a monomorphic appearance; apoptosis and mitosis are seen; necrosis is frequent. Inset: NUT IHQ showing a diffuse granular nuclear positivity.
No guidelines are available for the management and treatment of NC. Delayed diagnosis and refractory behavior to conventional therapy contribute to its poor prognosis. Clinicians and pathologists should consider NC in young patients with rapidly progressive thoracic masses and poorly differentiated carcinomas. Newer therapeutic options, mainly in BRD4-NUTM1 variants, are currently being evaluated.
Artificial Intelligence InvolvementNone of the material was produced with the help of any artificial intelligence software or tool.
Funding of the ResearchThis research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Conflicts of InterestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.