Primary trachea lymphoma is extremely rare, and the occurrence of primary Epstein Barr virus-positive (EBV+) diffuse large B-cell lymphoma (DLBCL) not otherwise specified (NOS) originating in the trachea is even rarer. Through literature review, we found that only three cases have been reported globally, and now we have identified the 4th case.
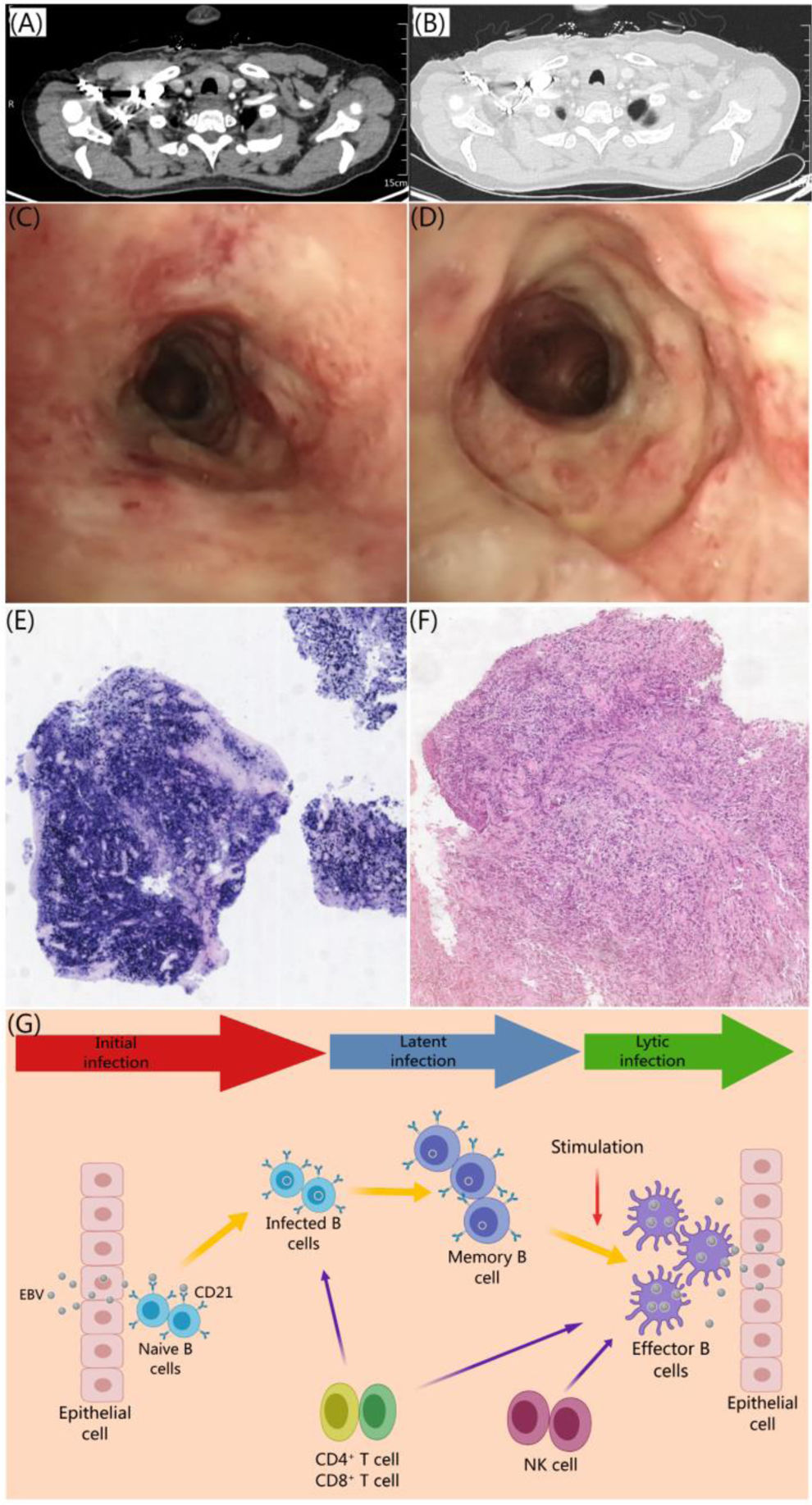
A 63-year-old woman presented with unexplained shortness of breath for the past 6 months. One month prior to her visit, she also experienced coughing, phlegm production, and coughing up blood, along with a weight loss of 1kg. She did not report any night sweats or fever and has no abnormal swellings in the superficial lymph nodes. A chest enhanced CT scan revealed multiple patchy high-density shadows in the upper lobe of the right lung, and rough tracheal wall. The bronchoscopy revealed protruding lesions and circumferential ulcerative lesions were seen in the main trachea. These lesions fused with each other, resulting in stenosis of the main trachea. There was a lot of pus fur on the surface. A biopsy was performed at the lesion site. The pathological results indicated that the main trachea was consistent with EBV+ DLBCL, NOS (Fig. 1).
(A and B) Enhanced CT scan of the chest reveals irregular tracheal wall. (C and D) There are protruding lesion and circumferential ulcer lesion in the main trachea that merge together. This merging has led to stenosis of the main trachea. Additionally, there is a large amount of pus coating on the surface. (E) Positive for EBER. (F) Diagnosed as diffuse large B-cell lymphoma. (G) Illustrates the initial infection of EBV.
Among the four cases of EBV-positive DLBCL, NOS, three were confirmed to had concurrent chronic diseases, such as Hashimoto's thyroiditis, diabetes mellitus, bronchogenic carcinoma, and lung infection. Treatment options for this condition include endoscopic surgery, conventional surgery, chemotherapy, and antibiotic therapy. Unfortunately, the prognosis is generally poor. One young patient passed away just two months after diagnosis due to a severe pulmonary infection, and chemotherapy was not accepted.1–3 EBV is the first virus to be identified as a tumor-associated virus. During primary infection, the innate immunity recognizes EBV and triggers an immediate antiviral response. This response then coordinates with the adaptive immunity to further combat the virus. To evade host immune surveillance and ensure the stability of the viral genome within the host, EBV employs various strategies to counteract the host's antiviral immune response (Fig. 1).
The early symptoms of primary tracheal EBV+ DLBCL-NOS are atypical, presenting with cough, chest tightness, and other respiratory symptoms. This disease is prone to misdiagnosis, and accurate diagnosis relies on bronchoscopy, multi-point biopsy, and pathological examination. Most patients present with tracheal stenosis, and surgical intervention or stent placement is crucial for managing acute respiratory distress. Combination chemotherapy and targeted therapy can partly improve the unfavorable prognosis, while the use of anti-PD-1 monoclonal antibodies in combination with R-CHOP can enhance efficacy and prognosis.4 Studies have shown that EBNA2 can by decreasing ICOSL through miR-24 reduces T cell activation to destroying tumor immunogenicity. Therefore, it is suggested that EBNA2+ patients might benefit the more from ICOSL-inducing therapy.5 Further prospective clinical studies are required to investigate the prognostic evaluation system and treatment strategies for this condition. It is highly recommended to actively enroll patients in clinical trials, seek biomarkers for predicting drug efficacy, and develop individualized treatment plans.
This work was supported by China Digestive Early Cancer Physicians Joint Growth Program Project (GTCZ-2020-SX-61-0001) and Shaanxi Province Key R&D Program General Project – Social Development Field (2024SF-YBXM-121).