Malignant sternal primitive tumours are rare and most constitute sarcomas. The incidence of radioinduced sarcomas of the chest wall is 0.2% at 10 years of treatment.1 Sternal resections are complex surgical procedures with potentially severe complications. The primary goal is radical oncological excision with adequate margins. Individualized assessment of the potential risks and benefits of these procedures is important, as well as multidisciplinary follow-up, with involvement of plastic surgeons. The available literature in terms of sternal resections is limited, heterogeneous and there is no consensus on optimal treatment.2 After chest wall disruption, the major challenge is to preserve respiratory function, with large defects requiring reconstruction to protect intrathoracic organs and restore physiological chest wall movements.3 A wide variety of reconstruction techniques using different materials have been described. Titanium has high corrosion resistance, low specific gravity and high tensile strength. It is biologically inert and has high biocompatibility.4 The literature describes various approaches for sternoclavicular joint ligaments restoration. It can be used autografts, allografts or synthetic. Given its fundamental stabilizing function and the lack of inherent osseous stability at this joint, surgical intervention with a focus on ligament reconstruction may be advised.5
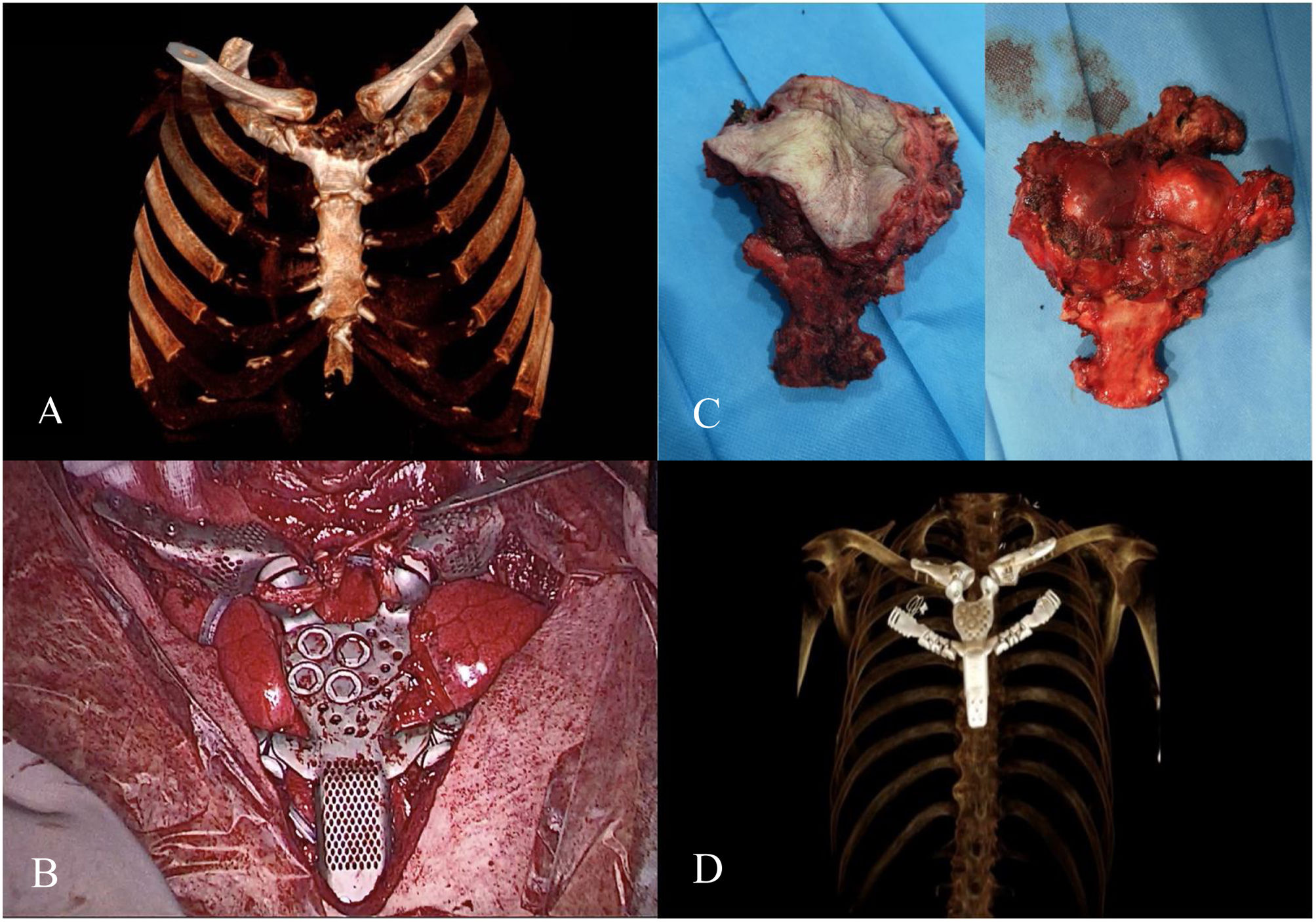
A 61-year-old male patient with a history of salivary gland adenocarcinoma (right radical parotidectomy) was treated with adjuvant chemoradiotherapy. Subsequent radiological controls revealed a lesion in the sternal manubrium with bone destruction suggestive of malignancy, with a diagnosis of high-grade fusocellular sarcoma (Fig. 1A). A radical surgery with curative intent was perfomed. For this purpose, 3D computed tomography reconstruction was planned. Along with biomedical engineers, a new type of personalized titanium implant was designed. Total sternectomy was performed, including the internal clavicular third with en bloc resection of soft tissue, paying attention to securing a 3-cm macroscopic margin of the bone. The customized titanium implant was fitted with metal suture cerclage on the costal edges. After a multidisciplinary committee evaluation, a mesh was not interposed between the implant and the underlying structures. The mesh infection could be a devastating complication due to devascularization and fibrosis after the previous radiotherapy received in the area for his previous neoplasia. The clavicular bone fixation was performed with screws. Subsequently, in order to create a sternoclavicular joint, it was assembled with perforated polyetheretherketone (PEEK) joint heads and cadaveric extensor tendons (Fig. 1B). Finally, with the collaboration of the plastic surgeons, the defect was covered with an anterolateral fasciocutaneous left thigh flap. There were no perioperative complications. He was discharged on the ninth postoperative day, with full joint mobility. Final pathology of the tumour was consistent with FNCLCC grade 3 radioinduced sarcoma, with free margins (Fig. 1C). Three months later, a body CT showed no evidence of recurrence and the integrated implant (Fig. 1D).
(A) 3D computed tomography reconstruction showing the radioinduced sternal sarcoma. (B) Customized dynamic titanium implant with sternoclavicular joint reconstruction. (C) Surgical resection specimen. (D) 3D computed tomography reconstruction showing correct positioning of the implant after surgery.
Radioinduced sarcomas are usually diagnosed in advanced stages. The majority of them are high-grade tumours. Therefore, early diagnosis is essential. Physiological reconstruction of the chest wall with custom-made titanium prosthetic material offers promising short-term results, emphasizing the functional thoracic reconstruction with biomechanically designed implants.
Conflict of interestsThe authors state that they have no conflict of interests.