Tuberculosis notification in Portugal has decreased in the last few years. As a consequence of the economic crisis, emigration has increased and immigration has decreased. Immigrants are a risk group for tuberculosis. Most emigrants are 20–44 years old and belong to the age group most affected by tuberculosis.
ObjectiveTo describe the decrease in tuberculosis notification in Portugal over the last years from a demographical point of view.
MethodsMathematical analysis was performed to quantify the effect of the migration movements (separately and simultaneously) on tuberculosis notification in Portugal from 2008 to 2014. We calculated the estimated tuberculosis notification for each year during the period of study: 1) fixing immigration rate and tuberculosis rate in immigrants at 2008 values; 2) fixing emigration rate and tuberculosis rate in emigrants at 2008 values; 3) fixing both phenomenons at 2008 values.
ResultsThe differences between the observed and the estimated numbers were small (≤0.5 cases/100000 inhabitants).
DiscussionImpact of the migration movements on tuberculosis notification rate does not seem to be significant when analyzed for each phenomenon individually and simultaneously, by our model. This might mean that we have to concentrate our efforts in other risk factors for tuberculosis.
La notificación de casos de tuberculosis en Portugal ha disminuido en los últimos años. Como consecuencia de la crisis económica, la emigración ha aumentado y la inmigración ha disminuido. Los inmigrantes son un grupo de riesgo para la tuberculosis. La mayoría de los emigrantes tienen entre 20 y 44 años y pertenecen al grupo de edad más afectado por la tuberculosis.
ObjetivoDescribir la disminución de la notificación de casos tuberculosis en Portugal en los últimos años, desde un punto de vista demográfico.
MétodosSe realizó un análisis matemático para cuantificar el efecto de los movimientos migratorios (por separado y simultáneamente) en la notificación de casos de tuberculosis en Portugal de 2008 a 2014. Se calculó la notificación de casos de tuberculosis estimada para cada año durante el período de estudio.
La notificación estimada de tuberculosis para cada año del periodo de estudio se calculó: 1) fijando las tasas de inmigración y de tuberculosis en inmigrantes con datos del año 2008; 2) fijando las tasas de emigración y de tuberculosis en emigrantes con datos del año 2008, y 3) fijando ambos fenómenos con datos del año 2008.
ResultadosLas diferencias entre los valores observados y los valores estimados fueron pequeñas (≤ 0,5 casos/100.000 habitantes).
DiscusiónSegún el modelo matemático propuesto en este trabajo, el impacto de los movimientos migratorios en la tasa de notificación de casos de tuberculosis en Portugal no parece ser significativo cuando se analiza cada fenómeno tanto individual como simultáneamente. Estos datos indicarían que deberíamos concentrar los esfuerzos en identificar otros factores de riesgo para la tuberculosis.
Since WHO declared tuberculosis (TB) a global emergency, many efforts have been made worldwide to decrease TB incidence.1 In Portugal, a TB National Programme was implemented in 1995 and in 2006 the “STOP TB strategy” was launched to delineate specific goals and strengthen the struggle towards the end of TB.2,3
Eight years later, in 2014, Portugal reached the threshold of low incidence, registering 20 new cases per 100000 inhabitants.4 Despite this, it remains the highest incidence country in the Western Europe and some areas still have an intermediate incidence. Lisbon and Oporto are the districts with the highest incidence.4,5
Homeless people, drug users, prisoners and migrants are at increased risk of developing TB. These groups concentrate in urban settings and their numbers tend to have an impact on TB.6-10 This work concentrates solely on the migrant movements’ effect on TB. In fact, in many European countries, most cases of tuberculosis occur within the immigrant population. About 26.8% of TB cases reported in the European Union (EU) and European Economic Area countries are of foreign origin.5 Therefore, migrants from high incidence countries have a considerable impact on the tuberculosis burden in low incidence countries.5,10 Increased risk of TB in this group might be related to higher exposure in the country of origin and/or worse socioeconomic conditions, comparing to the resident population.11
As opposed to other European countries, like Iceland, Cyprus, Norway or Sweden, where more than 70% of tuberculosis cases occur in foreign born individuals, in Portugal, this group represents only about 16% of cases.6,10,12 Nevertheless, TB incidence among immigrants in Portugal is much higher than in non-immigrants and it has been increasing.13
As a consequence of the economic crisis, in the last few years, an increasing number of individuals have left the country to live abroad. Portugal is the EU country with the largest number of emigrants per capita.14 In 2014, the number of emigrants had risen to the double, compared to 2008. The majority are young adults, aged 20–44 years old, that left Portugal seeking for better working and living conditions abroad.15,16 This age group overlaps with the one most affected by TB, between 25 and 54 years old.4
The main aim of this study is to describe the decrease in TB in Portugal over the last years purely from a demographical point of view. As such, the authors quantify the effect of the migration movements (immigration and emigration) on the TB notification in Portugal (from 2008 to 2014).
MethodsData and SourcesData on tuberculosis notification were collected from the Portuguese Tuberculosis Surveillance System (SVIG-TB) coordinated by the Directorate General of Health (DGH) during the seven year period ranging from 2008 to 2014. Data on migration movements for the period of study (2008-2014) were collected from Immigration and Borders Service Statistics and Statistics Portugal, the public Portuguese entity responsible for the official statistical information and included: 1) the absolute number of resident immigrants in each year; 2) the absolute number of immigrants entering the country per year; 3) the absolute number of emigrants per year; 4) the migration balance, which refers to the difference between the number of individuals entering and leaving the country, per year.
For the purpose of this paper, TB cases with no information on the country of origin were excluded from the analysis.
As this was a retrospective study and used routinely collected surveillance data, neither ethical approval nor informed consent were required.
Mathematical AnalysisThe impact of the migration movements on the TB burden was initially addressed separately for immigration and emigration, and simultaneously afterwards. The separate analysis allowed for the study of the influence of each migration phenomenon in isolation.
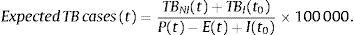
Firstly, the expected number of TB cases per 100000 inhabitants for year t (2008, 2009, …, 2014) under a steady situation of immigration (i.e., keeping both the number of immigrants and the number of TB-cases among immigrants at their 2008 values) was computed by:
Here, TBNI(t) denotes the number of TB-cases within the non-immigrant resident population in year t, TBI(t0) denotes the number of TB-cases within the immigrant population in t0=2008, and P(t) (resp. E(t), I(t0)) represents the number of Portuguese individuals (resp. emigrants, immigrants) in year t (resp. t, t0). Clearly, P(t)−E(t)+I(t0) corresponds to the total number of individuals resident in Portugal in year t.
Then, for each year, the expected number was compared with the observed number of TB-cases (including different annual counts for the number of immigrants and TB-cases among immigrants). The magnitude of the differences allowed for the evaluation of the impact of the immigration process on the TB incidence.
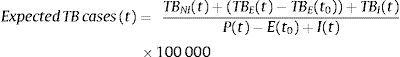
The model evaluating the impact of the emigration on TB in Portugal followed a similar reasoning; keeping both the number of emigrants and the number of TB-cases among emigrants at its 2008 value, the expected number of TB cases for year t per 100000 inhabitants was calculated by
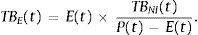
where the number of TB-cases among emigrants in year t, TBE(t), assumed the same per-capita rate as TBNI(t), namelyIndeed, had the TB-emigrants in year t stayed in the country and the difference TBE(t)−TBE(t0) would have been accounted for in the total number of cases within national territory. The magnitude of the differences between observed and expected counts allowed for the evaluation of the impact of the emigration process on the TB incidence.
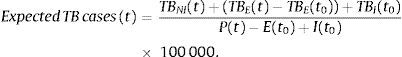
The study of the simultaneous effect of immigration and emigration combined the previous two equations. Under a steady scenario of immigration and emigration, the expected number of TB cases for year t per 100000 inhabitants would be
Finally, the relative annual fluctuations observed within the total number of Portuguese residents were compared with the relative annual decreases in the number of TB-cases. For each variable, the relative annual fluctuation between year t+1 and year t was computed as
ResultsFrom 2009 to 2013 there was a steady annual increase in the number of emigrants and essentially a decrease in the number of immigrants. The years 2008 and 2014 have slightly contradicted this trend.
Until 2010, the number of immigrants per year was higher than the number of emigrants. From 2011 to 2014, there was an inversion in the migration flow, and the number of emigrants exceeded the number of immigrants, thus turning the migration balance negative (Table 1).
Migration Movements.
| Year | Total resident population N | Resident inmigrants N | Emigrants N | Immigrantsa N | Migration balanceb | Portuguese individualsc N |
|---|---|---|---|---|---|---|
| 2008 | 10563014 | 440277 | 20357 | 29718 | 9361 | 10553653 |
| 2009 | 10573479 | 454191 | 16899 | 32307 | 15408 | 10558071 |
| 2010 | 10572721 | 445262 | 23760 | 27575 | 3815 | 10568906 |
| 2011 | 10542398 | 436822 | 43998 | 19667 | −24331 | 10566729 |
| 2012 | 10487289 | 417042 | 51958 | 14606 | −37352 | 10524641 |
| 2013 | 10427301 | 401320 | 53786 | 17554 | −36232 | 10463533 |
| 2014 | 10374822 | 395195 | 49572 | 19516 | −30056 | 10404878 |
M: male; F: female.
The number of TB cases has been consistently decreasing since 2008. Cases occurring in immigrants represented 13.8% of all cases in 2008, 15.2% in 2009 and remained stable at about 16% since 2010. Immigrants have a much higher notification rate of TB than the Portuguese individuals (Table 2).
Tuberculosis Numbers.
| Year | TB casesa N | TB rateb | TBPIc N | TBPI rated | TBIe N | % TBI | TBI ratef | TB cases missing origin N (%) |
|---|---|---|---|---|---|---|---|---|
| 2008 | 2967 | 27.8 | 2523 | 23.9 | 410 | 13.8 | 93.1 | 34 (1.2) |
| 2009 | 2869 | 27.1 | 2432 | 23.0 | 437 | 15.2 | 96.2 | 0 (0) |
| 2010 | 2714 | 25.6 | 2273 | 21.5 | 438 | 16.1 | 98.4 | 3 (0.1) |
| 2011 | 2609 | 24.7 | 2203 | 20.9 | 404 | 15.5 | 92.5 | 2 (0.1) |
| 2012 | 2606 | 24.6 | 2176 | 20.7 | 408 | 15.7 | 97.8 | 22 (0.8) |
| 2013 | 2399 | 22.8 | 1989 | 19.0 | 393 | 16.4 | 97.9 | 17 (0.7) |
| 2014 | 2264 | 21.8 | 1904 | 18.3 | 357 | 15.8 | 90.3 | 3 (0.1) |
M: male; F: female; TB: tuberculosis.
Similar to the TB notification rate, the total resident population in Portugal, has essentially decreased over 2008–2014 (with the exception of a slight increase from 2008 to 2009). However, the relative annual decrease on the number of residents was lower than the decrease on the TB numbers (Table 3).
As shown in Table 1, from 2008 to 2014 there were relatively few immigrants entering Portugal. Fixing both the immigration rate and the TB rate among immigrants at their 2008 values, and considering the variation on emigration that has actually occurred, we’ve estimated the number of TB cases per 100000 inhabitants for each studied year (Table 4). The differences between the observed and the estimated numbers were residual, ranging from more 0.27 cases/100000 inhabitants in 2010 to less 0.49 cases/100000 inhabitants in 2014.
Differences Between Observed and Estimated Numbers of TB Cases When Evaluating the Impact of the Immigration on the TB Notification Rate.
| Year | Observed number of TB cases per 100000 in inhabitants (O) | Expected TB cases per 100000 inhabitants (E) | O−E |
|---|---|---|---|
| 2008 | 27.77 | NA | NA |
| 2009 | 27.13 | 26.89 | 0.24 |
| 2010 | 25.64 | 25.37 | 0.27 |
| 2011 | 24.73 | 24.76 | −0.03 |
| 2012 | 24.64 | 24.62 | 0.02 |
| 2013 | 22.84 | 22.98 | −0.14 |
| 2014 | 21.79 | 22.28 | −0.49 |
O: observed; E: expected.
On the other hand, emigration rose significantly during the period of study (Table 1), which could have influenced the TB rate in the country to go lower.
The official number of TB cases in emigrants leaving the country in 2008 was 4.87/100000 inhabitants. Assuming that this rate remained constant along 2008–2014 and that the total number of emigrants did not change either along that period, we estimated annual numbers for TB in Portugal. The observed numbers were only slightly higher than their estimates. The differences were even smaller than those found for the immigration impact (<0.1 cases/100000 inhabitants) (Table 5).
Differences Between Observed and Estimated Numbers of TB Cases When Evaluating the Impact of the Emigration on the TB Notification Rate.
| Year | Observed number of TB cases per 100000 in inhabitants (O) | Estimated TB cases per 100000 inhabitants (E) | O−E |
|---|---|---|---|
| 2008 | 27.77 | NA | NA |
| 2009 | 27.13 | 27.13 | 0.00 |
| 2010 | 25.64 | 25.64 | 0.00 |
| 2011 | 24.73 | 24.71 | 0.02 |
| 2012 | 24.64 | 24.62 | 0.02 |
| 2013 | 22.84 | 22.82 | 0.02 |
| 2014 | 21.79 | 21.77 | 0.02 |
O: observed; E: estimated.
When looking at both migration movements at the same time, the observed TB rate was again identical to the estimated TB rate (differences between less 0.43 cases/100000 inhabitants in 2014 and more 0.28 cases/100000 inhabitants in 2010) (Table 6).
Differences Between Observed and Estimated Numbers of TB Cases When Evaluating Simultaneously the Impact of Immigration and Emigration on the TB Notification Rate.
| Year | Observed number of TB cases per 100000 in inhabitants (O) | Estimated TB cases per 100000 inhabitants (E) | O−E |
|---|---|---|---|
| 2008 | 27.77 | NA | NA |
| 2009 | 27.13 | 26.89 | 0.24 |
| 2010 | 25.64 | 25.36 | 0.28 |
| 2011 | 24.73 | 24.71 | 0.02 |
| 2012 | 24.63 | 24.55 | 0.08 |
| 2013 | 22.84 | 22.91 | −0.07 |
| 2014 | 21.79 | 22.22 | −0.43 |
O: observed; E: estimated.
The number of TB cases has been decreasing in Portugal (notification rate was 27.8/100000 inhabitants in 2008 vs 21.8 cases/100000 inhabitants in 2014). Since 2009, the resident population has also been decreasing, but at a slower pace, as shown in Table 3. As for that, the decreasing number of TB cases cannot only be due to the reduction in the resident population.
Between 2008 and 2010, the number of immigrants exceeded the number of emigrants (positive migration balance). Since 2011 until 2014, migration balance turned negative. Moreover, TB rate has been consistently higher among immigrants compared to the native population (>90 cases/100000 inhabitants vs 18.3–23.9 cases/100000 inhabitants). The percentage of TB cases in this group has risen from 13.2% in 2008 to 15.2% in 2009 and remained at about 16% since 2010. This model allowed us to evaluate the impact of the immigration on the TB rate. It showed that, since 2011, as immigration is decreasing, there is a tendency to a lower number of TB cases. However, the differences are very small, representing less than 1 case per 100000 inhabitants, so the impact does not seem to be significant.
A decrease in TB incidence has been the trend in the whole WHO European Region over the last years, where it has fallen by 5.2% each year, since 2005.5
Efforts have been made to achieve lower TB rates in Europe, even in low incidence countries. Out of 31 low incidence countries evaluated, more than half (54.8%) reported to have a dedicated national TB programme.17
Despite this global trend and even though we failed to demonstrate a significant impact of the immigration global decrease on TB rate, immigrants are still a risk group as in many of their origin countries, infectious diseases, such as TB, are still an important cause of death and morbidity.18
In low incidence countries, the impact of immigration on the burden of TB has been largely studied.10,19-21 Addressing risk groups is one of the key strategies against TB.8,22
In the recently published action framework of the WHO towards TB elimination in low incidence countries23 strategies involving migrants are mentioned in three of the eight priority action areas: 1) to address the most vulnerable and hard-to-reach groups; 2) to address special needs of migrants and crossborder issues and 3) to undertake screening for active TB and latent tuberculosis infection (LTBI) in TB contacts and selected high-risk groups, and provide appropriate treatment.
Many efforts have been made to detect TB and LTBI among migrants.12 Some EU countries have implemented screening of migrants before, or at entry.24 Underwood et al. compared contact tracing with new entrant screening in London and found the former to be more effective, as it identifies families and communities at high risk.21 With the recent increase in the number of immigrants coming to Europe as refugees (rising from about 219000 in 2014 to more than one million in 2015), TB control in this group is also a concern.25,26 Regarding this matter, the ERS/WHO European Region has performed a study in order to document the policies and practices of low and intermediate TB incidence European countries with regards to detection and management of TB and latent TB infection among this vulnerable group.26
In countries where most cases of TB occur in foreign born individuals or where incidence in this group is increasing, despite a decreasing TB rate, as it occurs in Portugal, policies on this subject are of great importance.
As for the emigration increase over the period of study, our model showed very little differences between the number of observed and expected cases (<0.1 cases/100000 inhabitants each year). The fact that the differences between observed and expected cases were smaller than those found for the immigration impact can mean that the increase in emigration that we observed over 2008–2014 has not significantly impact the national TB rate.
We assumed the TB rate in emigrants to be similar to the TB rate in the Portuguese individuals that stayed in the country. However, we do not know if these individuals had other risk factors for TB or if they became more vulnerable for TB when they moved abroad.
Torres Redondo et al.27 retrospectively analyzed the Portuguese emigrants diagnosed with TB when returning to the country, in the Northern Region in 2014. Most cases (76.3%) had moved to low TB incidence countries and had lived there for more than 2 years (median time of 42.0 months), which could suggest that exposure to TB could have already occurred in the foreign country. About 67% shared housing with work colleagues. These data suggest that risk for TB might increase when emigrants leave the country as they might experience harder living conditions and economic adversity. Nevertheless, had they stayed in the country they might have been unemployed which also accounts as a risk factor for TB.28
Despite the lack of knowledge about this group, our model failed to demonstrate an impact of emigration on TB notification rate.
Individually, the migration movements did not influence TB rate when analyzed by our model, so we tried to look at the impact of both movement altogether. Differences were again very small (<0.5 cases/100000 inhabits each year), so, even when combined, migration movements do not seem to largely influence TB notification rate.
This might mean that we have to concentrate our efforts in other risk factors. Sousa et al.28 recently found HIV to be the factor with this highest impact: an increase of 10 HIV notifications per 100000 inhabitants was associated with a rise of 2 new TB cases per 100000 inhabitants. Also, an increase of 1000 unemployed subjects per 100000 inhabitants was associated with one new case of TB per 100000 inhabitants.
Apart from HIV infection, poor living and working conditions, which can facilitate TB transmission and risk factors that impair host's defense, like malnutrition, smoking, diabetes, alcohol abuse and indoor air pollution have been pointed out as major determinants.29-32Silicosis also increases the risk of TB by 2.8–39 times.33,34 Silico-TB can be a challenging diagnosis and treatment must be longer.35
Preventive strategies that target these factors might have an important impact on TB burden.
These risk factors also add to the risk for TB in the migrant population. Paulino et al.13 found that foreign born patients were more likely to be HIV positive, to be employed, homeless or live in shelters. Reducing HIV infection and providing better living conditions might have an even greater impact on TB among migrants. A study performed in Italy by Ingrosso et al. also showed that HIV infection is three times more frequent in foreign born people affected by TB than among Italians.36
Altogether, these factors represent areas of intervention towards TB elimination and should all be addressed in national and international TB programmes.23
In this work, the authors tried to understand the impact of two demographic factors – the migration movements and the decrease in the total number of residents – on the burden of TB in Portugal over the 7-year period 2008–2014. As such, other risk factors such as HIV infection, homelessness or overcrowded housing were assumed to remain constant over that period.
In conclusion, the changing pattern of migration in Portugal over the period of study (2008–2014) does not seem to have had a significant impact on the TB notification rate.
AuthorshipAll authors contributed to drafting and review of the manuscript.
Conflict of InterestThe authors declare to have no conflict of interest directly or indirectly related to the manuscript contents.
Rita Gaio was partially supported by CMUP (UID/MAT/00144/2013), which is funded by FCT (Portugal) with national (MEC) and European structural funds (FEDER), under the partnership agreement PT2020.
This work was supported by the contribution of Iceland, Liechtenstein and Norway, through the EEA Grants, under the Public Health Initiatives Programme (PT 06), grant number 138DT1.