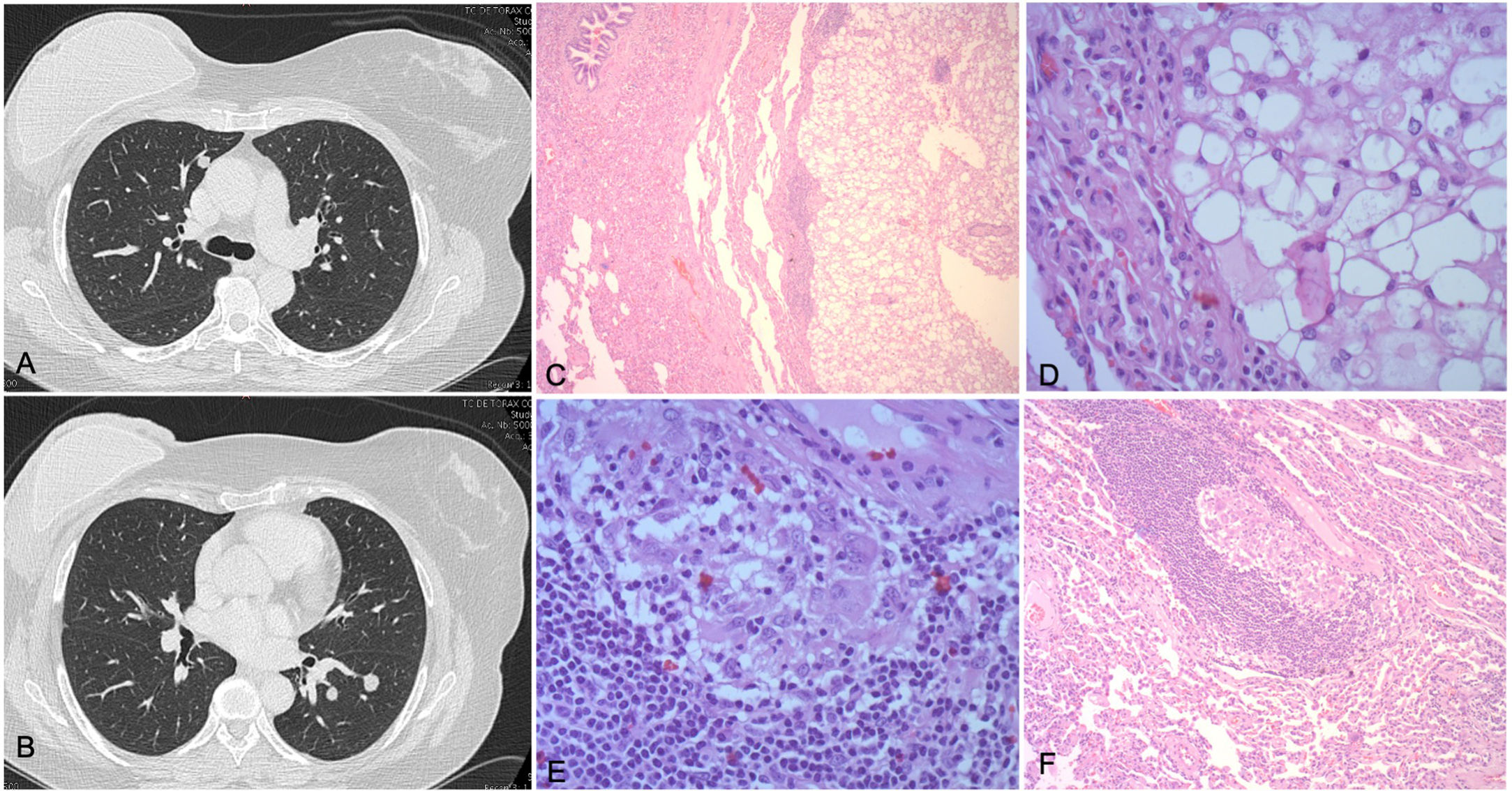
A 52-year-old woman with stage IA infiltrating lobular breast cancer underwent right radical mastectomy with immediate reconstruction. In her oncological follow-up, a cannonball radiological pattern was observed (Fig. 1), so one of the nodules was biopsied for histologic typing.
(A–B) Pre-operative CT image showing bilateral pulmonary nodules. A) Subpleural pulmonary nodule in the anterior segment of the right upper lobe. B) Left lower lobe pulmonary nodules. (C–F) Histologic images of the pulmonary nodule resected during surgery. C) Pulmonary parenchyma and bronchiole observed on the left, and on the right a nodule consisting of cells that appear light-colored at this magnification, with an incomplete lymphocytic rim (a foreign body granuloma variant). D) At higher magnification, these cells are seen to be histiocytic with a large “blank”, i.e. empty cytoplasm, because the silicone dissolves as it is processed, leaving a hollow space. E) Foreign body granuloma in the lung parenchyma near a vein. F) At higher magnification, the typical histiocytes and multinucleated giant cells are seen in more detail.
Atypical right S3 segmentectomy was performed by video-assisted thoracoscopy and, surprisingly, an intra-pulmonary nodule was reported, consisting of intra-cytoplasmic oily material with a lymphocytic rim, with the presence of giant cell microgranulomas with intravascular oily material, consistent with a diagnosis of pulmonary siliconoma (Fig. 1).
A conservative approach was taken with regard to the nodules (as resection would have required a lobectomy), with close follow-up and replacement of the silicone implant, which was assumed to have ruptured. No changes in the lung lesions were observed in successive follow-ups.
In 1964, Winer first described siliconoma (foreign body granulomatous reaction caused by liquid silicones in the tissues and surrounding fibrosis). Late complications, such as local siliconomas or lymphadenopathies, are widely described, while peripheral spread to subcutaneous tissue and the existence of intrapulmonary siliconomas are extremely rare. We have only found reports by Muñiz et al.1 and Dragu et al.2, which, unlike our case, were single lung lesions.
Conflict of interestsAll authors declare no conflict of interests.
This study received no specific grants from public sector agencies, the commercial sector, or from non-profit organizations.
Please cite this article as: Cózar Bernal F, González Fernández J, Girón Arjona JC, Siliconoma pulmonar, una etiología a tener en cuenta. Arch Bronconeumol. 2022;58:83.