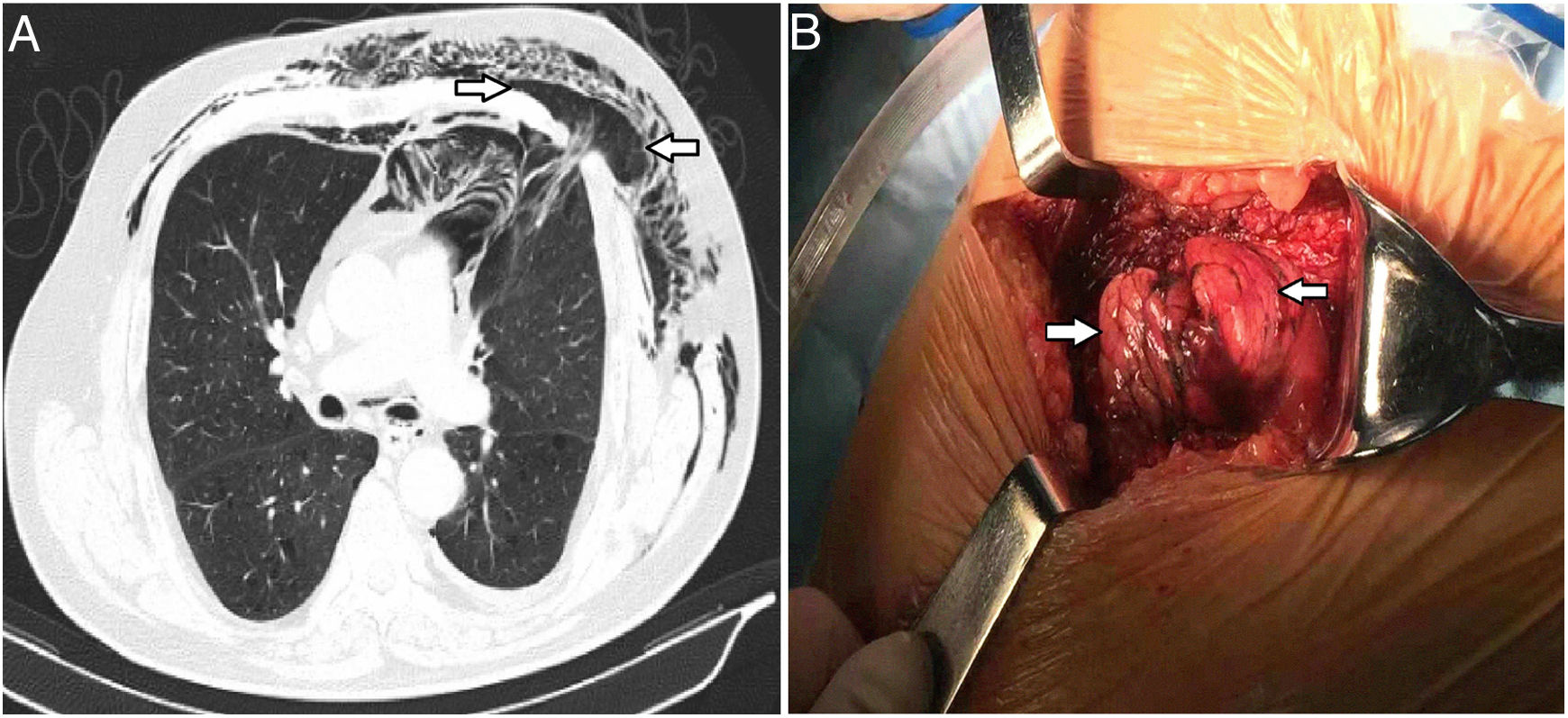
A 63-year-old man with a 4-day history of pain in the left side of the chest that had begun after an episode of severe coughing presented to the emergency department with dyspnea. He described that swelling became more prominent on coughing on the left side of the chest. He had a history of smoking and drinking for 40 years. There was no history of chest surgery or traveled to Wuhan, having been no close contact with patients with coronavirus disease 2019 (COVID-19). His clinical manifestations were compatible with COVID-19 and the initial oxygen saturation was only 89% while he was breathing ambient air. The chest X-ray from the local hospital showed ground-glass opacities (GGO) in peripheral zones of left upper lobes, extension of lung parenchyma beyond the rib cage. However, throat swab samples were collected and tested negative for SARS-CoV-2. A CT imaging from our hospital showed pneumonia, subcutaneous emphysema, pneumomediastinum and a large intercostal lung herniation (arrows) in the left second intercostal space (Fig. 1). To our knowledge, spontaneous lung herniation is a rare entity.1 The surgery was completed by fixing the ribs outside the thoracic wall with 2–0 nylon suture and defect closed. After the procedure, the patient recovered well. A repeated chest CT scan showed the previous GGO were significantly reduced. The patient was discharged home.
Intercostal lung herniation (arrows). (A) CT scan revealed pneumomediastinum, a small pneumothorax, subcutaneous emphysema and a focal intercostal muscle defect in the second intercostal space, with lung and pleural herniation (arrows). (B) Thoracic surgery with marked lung herniation (arrows).
This study was financially supported by the Science & Technology Program of Tianjin First Central Hospital (Grant Nos. CM201803 and CF201807).
Conflict of interestThe authors have no conflicts of interest to disclose