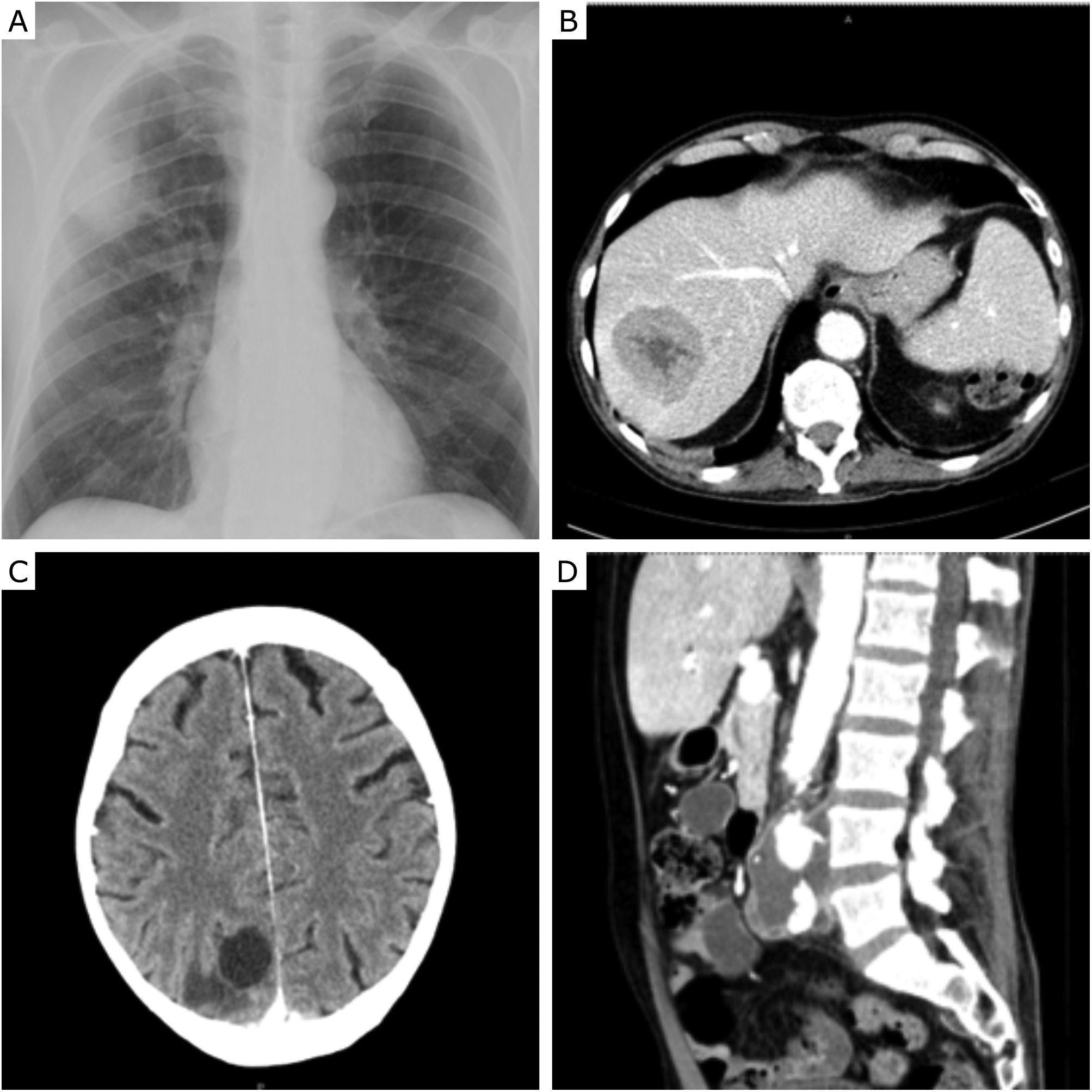
62-Year-old male, smoker (100 Pack-year), presented with dry cough and dizziness within the past 3 week, being hospitalized after detecting a lung mass in the right upper lobe in the chest X-ray (Fig. 1A). CT scan confirmed the presence of the lung mass, also identifying bilateral lung nodules, mediastinal adenopathies, and a hepatic nodule (Fig. 1B). Cranioencephalic CT scan found multiple brain nodules, associated with vasogenic oedema (Fig. 1C). A transthoracic needle biopsy was performed, identifying a lung adenocarcinoma with negative molecular study and PD-L1 of 1–5%.
(A) Chest X-ray showing a mass in the right upper lobe; (B) hepatic nodule identified in the abdominal CT scan; (C) cranioencephalic CT scan with the presence of a nodule in the occipital area, with vasogenic oedema; (D) abdominal CT scan showing a thrombosed aneurysm in the abdominal aorta.
The patient was discharged and 3 weeks later he presented with asthenia, haematuria, constipation, and jaundice. Laboratory tests revealed severe macrocytic anaemia with 4.2g/dL haemoglobin (13.5g/dL haemoglobin at discharge), and leucocytosis in the complete blood count. Elevated levels of LDH (1069UI/L), bilirubin (6mg/dL), and C-reactive protein (362mg/dL) were also found. After evaluation by immunohemotherapy, irregular antibody screening was positive, with a positive direct Coombs test and C3d monospecific test. These results sustained the diagnosis of an autoimmune haemolytic anaemia due to cold agglutinin syndrome. The patient was started on antibiotics, in addition to corticotherapy, IV immunoglobulin on 2 consecutive days, and transfusion of 4 units of heated red blood cell concentrates, while maintaining body temperature above 35°C. Blood and urine cultures identified Methicillin-Sensitive Staphylococcus aureus (MSSA).
Two weeks after being discharged, the patient presented asthenia, anorexia, and joint pain. Blood cultures were again positive for MSSA, and an abdominal CT identified a thrombosed abdominal aortic aneurysm (Fig. 1D), where a possible lodging for the bacteria was suspected. After two cycles of antibiotics, blood cultures were negative and haemoglobin values were stable after transfusing one unit of heated red blood cell concentrate. Chemotherapy with Carboplatin and Pemetrexed was started during hospitalization. After this episode, the patient experienced sudden pain and swelling in his left leg. Echo-doppler identified thrombi in the deep veins bilaterally, causing subtotal obliteration on the right side and complete on the left. Analytically, he presented pancytopenia, requiring a new transfusion under steroid therapy and IV immunoglobulin. Chemotherapy was later changed to Vinorelbine, administering the first cycle during hospitalization. There was a progressive deterioration in the patient's general condition, culminating in anuria and prostration one month after the last hospitalization, ultimately leading up to the patient's death.
Paraneoplastic syndromes are rare disorders in patients with solid tumours, triggered by remote effects of the tumour, such as an ectopic production of biological substances or by abnormal immune system response to the tumour.1,2 Autoimmune hemolytic anaemia is a known paraneoplastic phenomenon.3 Cold agglutinin syndrome is a rare type of autoimmune hemolytic anaemia, produced by antibodies that react at low temperatures with the patient's own erythrocytes, destroying them. This syndrome is mostly associated with lymphoproliferative disorders, although there have been reported cases of paraneoplastic cold agglutinin syndrome associated with solid tumours, including lung adenocarcinoma.4,5
In this case, the appearance of this syndrome triggered frequent complications, leading to a deterioration of the patient's general condition and several hospitalizations, which made the approach and treatment of the neoplasia very challenging.
FundingThere is no funding related to this article.
Conflict of interestsThe authors state that they have no conflict of interests.