Our patient, a 56-year-old man, underwent surgery for esophageal adenocarcinoma, involving esophagectomy with intrathoracic esophagogastric anastomosis. After the procedure, the patient developed anastomotic stenosis that was refractory to multiple dilation procedures, so after 1 year of follow-up we decided to implant a covered metallic stent. After the intervention, the patient developed a persistent cough, leading to the finding of a bronchogastric fistula. After 6 months of follow-up, recurrent symptoms of esophageal stenosis required stent replacement.
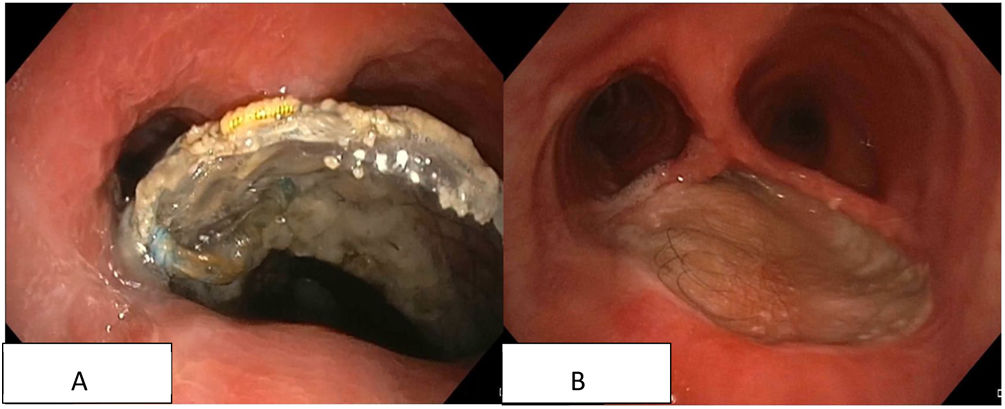
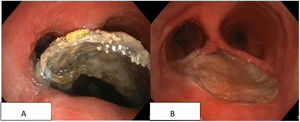
In the follow-up bronchoscopies, a distal shadow was observed in the pars membranacea of the trachea extending to the right main bronchus. The patient's clinical situation deteriorated, with excessive salivation and irritative cough on ingestion, so a chest computed tomography (CT) scan and bronchoscopy were performed, which revealed that the stent had migrated to the distal third of the trachea, ruptured the pars membranacea, and emerged above the main carina (Fig. 1A, video). Finally, with the collaboration of the plastic surgery and thoracic surgery departments, we performed total gastrectomy, closure of the tracheal defect with left radial myocutaneous flap,1 and coloplasty (Fig. 1B, video). Currently, 36 months after the intervention, the patient is undergoing regular endoscopic monitoring that shows a well-positioned graft with no gut-airway communication.