Jet ventilation, a technique involving intermittent occlusion of airflow from a high-pressure source through a pneumatic or electronically controlled interruption device, generates a tidal volume (VT) through a combination of driving airflow and entrained air via the Venturi effect, a phenomenon where high-speed airflow draws in surrounding air.1 Key clinical variables include ventilation frequency (F), driving pressure (DP), inspiratory-to-expiratory ratio (I:E), and the angle and entry depth of jet needle. The resultant VT to the lungs is influenced by factors such as the volume of the driving gas, the efficiency of Venturi entrainment, and the physiological condition of the lungs.2,3 Monitoring ventilation, especially airway pressure and carbon dioxide level, poses challenges, potentially leading to inadequate or excessive ventilation.4 Inadequate ventilation can result in hypoxemia and hypercapnia, while prolonged exposure to high tidal volumes increases the risk of volume–pressure-related lung injury.5
VT is not directly adjustable and results from the interplay of factors such as DP, jet needle (casing) resistance, inspiratory time, entrainment volume, and respiratory system impedance (lung compliance, tracheal resistance).6 Notably, the inner diameter (ID) of the jet needle is overlooked in clinical practice, with no industry standards referencing its importance.
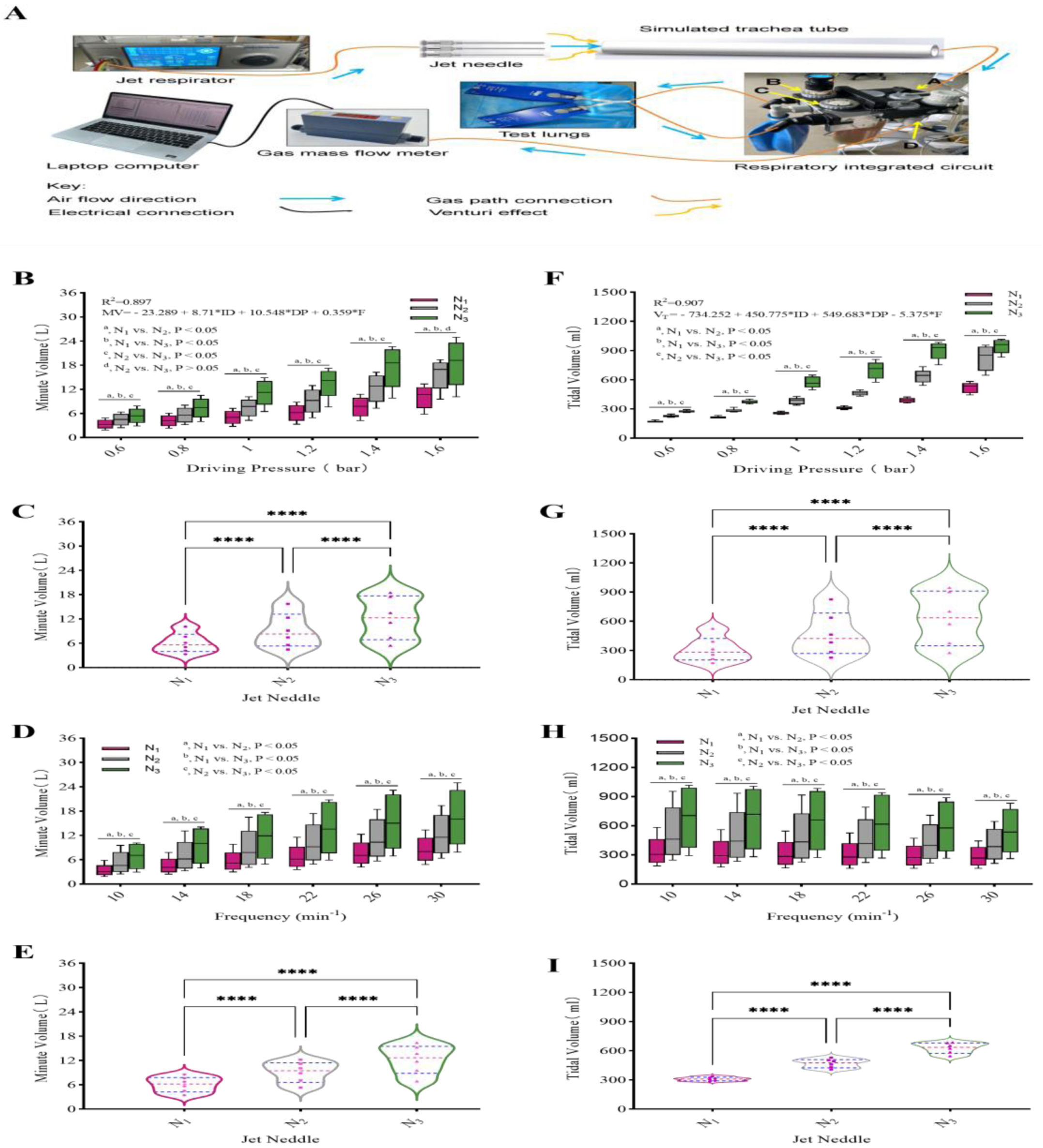
In this study, a jet ventilator (TwinStream™, Austria) connected to the normal-frequency jet tube, creating a link to a simulated airway (PE plastic pipe with a ID of 14mm and a length of 20cm). Three types of needles (ID: N1=1.2mm, N2=1.6mm, N3=1.9mm) with lengths of 25mm were selected. The one-way valve function of the DrägerFabius anesthesia machine's integrated air circuit (Germany) was utilized and connected to a simulated lung (DrägerSelfTestLung™, Germany, compliance: 45mL/cmH2O). A gas-collecting plastic bag was utilized to collect exhalation flow, and the gas volume was quantified using a high-precision industrial flowmeter (MF/FS4000, USA) (Fig. 1A). Six distinct frequencies (10, 14, 18, 22, 26, 30min−1) were examined under six different DPs (0.6, 0.8, 1.0, 1.2, 1.4, 1.6bar). Each parameter setting was replicated five times per group.
Significant differences were observed in both the MV and VT among the three types of jet needles under identical parameter settings. (A) Schematic diagram of experimental set-up. The respiratory circuit diagram includes the following components, as indicated by the legend: (A) the interface for the suction line; (B) the one-way valve for suction; (C) the one-way valve for expiration; and (D) the exhaust outlet. (B–E) Perform a comparative analysis of minute ventilation in response to varying drive pressures and frequencies for the three needles. (F–I) Perform a comparative analysis of tidal volume in response to varying drive pressures and frequencies for the three needles.
SPSS version 26.0 and GraphPad Prism 9 software were employed for statistical analyses and to facilitate the comparison of findings. Upon maintaining a consistent DP, a significant difference (P<0.05) was observed in both the MV and VT across three needles at six frequencies (with the exception of DP=1.6bar, N2 vs. N3, P>0.05) (Fig. 1B and F). When operating at the same frequency, both the MV and VT exhibited significant differences across three needles at six DPs (P<0.05) (Fig. 1D and H). Multiple linear regression analysis revealed significant effects of DP, needle diameter, and frequency on both MV and VT (P<0.0001) (Fig. 1B and F).
Literature on jet ventilation commonly reported the use of experimental jet needles with varying inner diameters, ranging from 0.7 to 3mm, exhibiting considerable variability.7–9 Regardless of whether an adaptor for the jet ventilator or a laryngoscope equipped with jet ventilation capabilities is employed, the IDs of the integrated jet needles are not uniform.10–12 Whether utilizing an adaptor for the jet ventilator or a laryngoscope equipped with jet ventilation is a consistent challenge. Drawing from the simplified Bernoulli equation for an ideal gas (P+(1/2)ρV2=normal, where P represents pressure, ρ denotes density, and V signifies velocity), we observed that a reduction in the ID of the injection needle correlates with an increase in flow velocity, assuming a normal DP – consequently, a smaller ID results in higher flow velocities.13 Applying Poiseuille's law (Q=π×r4×Δp (8ηL)−1, where Q is the volume flowrate, r is the radius of the pipe, Δp is the pressure difference, η is the fluid viscosity, and L is the length of the pipe), gas flow is primarily dependent on the ID of the injection needle when the DP and suction time are normal.14 A larger ID corresponds to an increased gas flow. Therefore, variations in the ID of the injection needle, while holding other parameters normal, result in different velocities and flow rates of ejected air, subsequently impacting ventilation effectiveness in a simulated lung model. Previous studies have suggested that a reduction in the ID of the jet needle correlates with a decrease in the VT under identical setting parameters.15 The findings of the current study are consistent with those reported in the literature.
For a given jet needle, we found that VT exhibited a positive correlation with DP and an inverse correlation with frequency. Conversely, MV demonstrated a positive correlation with both DP and frequency. During the breathing cycle, a shorter inspiratory phase results in both a reduced jet-driven volume and a decreased entrainment volume, leading to a lower VT. As the frequency escalates, the inspiratory time correspondingly contracts. According to the law of conservation of energy, the potential energy of the airflow in each respiratory cycle decreases, evident in a decline in VT. This phenomenon is attributed to the relationship between frequency and the volume of gas delivered. While the volume of gas administered per minute remains normal, increased frequency results in a reduced volume of gas per breath. Consequently, the entrained volume of gas decreases in tandem with the volume per respiratory cycle.
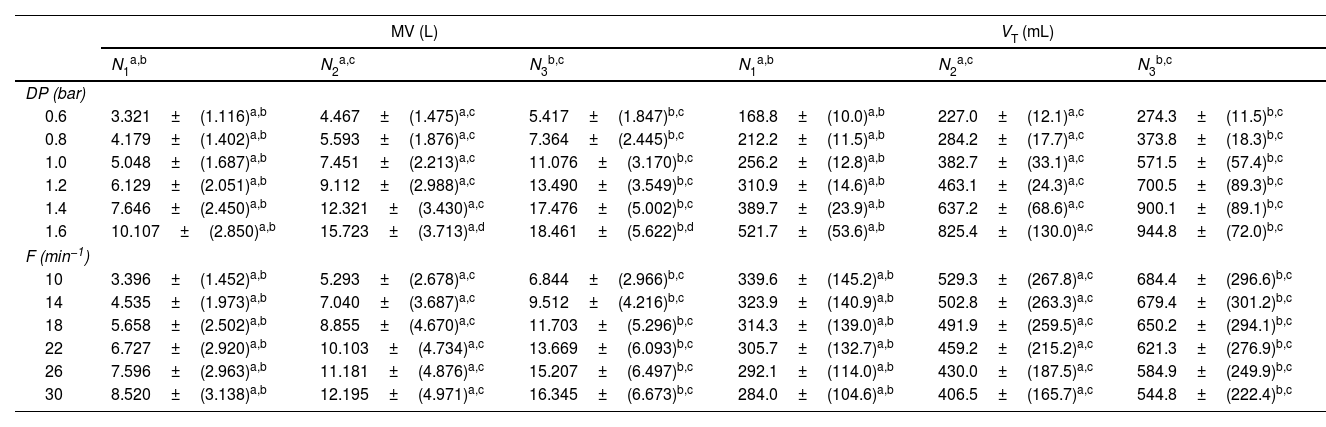
Upon reaching a driving pressure of 1.6bar, the VTs generated by injection needles N2 and N3 both exhibited a ceiling effect, with no statistically significant difference observed in MV (Table 1 and Fig. 1B). This outcome suggests that in target lungs jet ventilation, needles with larger diameters more readily approach the physiological ventilation limit. Consequently, any further increase in driving pressure may result in volumetric lung injury. When employing a jet needle with a larger ID and high DP to a normal adult, accurately evaluating the MV and VT excursion visually can become challenging for an anesthesiologist. Prolonged ventilation with high VT has the potential to lead to ventilator-associated acute lung injury (VILI) and hyperventilation.9 Consequently, vigilance is imperative in this regard. While obesity is often considered a relative contraindication for jet ventilation, certain studies have reported successful use of high DP (4bar) in obese patients (BMI≥30).16 This success may be attributed to the increased DP and resultant higher VT associated with jet ventilation.
Comparison of Minute Volume (MV) and Tidal Volume (VT) Among Three Types of Jet Needles in Jet Ventilation. The Applied Driving Pressure (DP) Ranged From 0.6 to 1.6bar, While the Frequency (F) Varied From 10 to 30 Cycles per Minute. Data are Presented as Mean±Standard Deviation (n=6).
| MV (L) | VT (mL) | |||||
|---|---|---|---|---|---|---|
| N1a,b | N2a,c | N3b,c | N1a,b | N2a,c | N3b,c | |
| DP (bar) | ||||||
| 0.6 | 3.321±(1.116)a,b | 4.467±(1.475)a,c | 5.417±(1.847)b,c | 168.8±(10.0)a,b | 227.0±(12.1)a,c | 274.3±(11.5)b,c |
| 0.8 | 4.179±(1.402)a,b | 5.593±(1.876)a,c | 7.364±(2.445)b,c | 212.2±(11.5)a,b | 284.2±(17.7)a,c | 373.8±(18.3)b,c |
| 1.0 | 5.048±(1.687)a,b | 7.451±(2.213)a,c | 11.076±(3.170)b,c | 256.2±(12.8)a,b | 382.7±(33.1)a,c | 571.5±(57.4)b,c |
| 1.2 | 6.129±(2.051)a,b | 9.112±(2.988)a,c | 13.490±(3.549)b,c | 310.9±(14.6)a,b | 463.1±(24.3)a,c | 700.5±(89.3)b,c |
| 1.4 | 7.646±(2.450)a,b | 12.321±(3.430)a,c | 17.476±(5.002)b,c | 389.7±(23.9)a,b | 637.2±(68.6)a,c | 900.1±(89.1)b,c |
| 1.6 | 10.107±(2.850)a,b | 15.723±(3.713)a,d | 18.461±(5.622)b,d | 521.7±(53.6)a,b | 825.4±(130.0)a,c | 944.8±(72.0)b,c |
| F (min−1) | ||||||
| 10 | 3.396±(1.452)a,b | 5.293±(2.678)a,c | 6.844±(2.966)b,c | 339.6±(145.2)a,b | 529.3±(267.8)a,c | 684.4±(296.6)b,c |
| 14 | 4.535±(1.973)a,b | 7.040±(3.687)a,c | 9.512±(4.216)b,c | 323.9±(140.9)a,b | 502.8±(263.3)a,c | 679.4±(301.2)b,c |
| 18 | 5.658±(2.502)a,b | 8.855±(4.670)a,c | 11.703±(5.296)b,c | 314.3±(139.0)a,b | 491.9±(259.5)a,c | 650.2±(294.1)b,c |
| 22 | 6.727±(2.920)a,b | 10.103±(4.734)a,c | 13.669±(6.093)b,c | 305.7±(132.7)a,b | 459.2±(215.2)a,c | 621.3±(276.9)b,c |
| 26 | 7.596±(2.963)a,b | 11.181±(4.876)a,c | 15.207±(6.497)b,c | 292.1±(114.0)a,b | 430.0±(187.5)a,c | 584.9±(249.9)b,c |
| 30 | 8.520±(3.138)a,b | 12.195±(4.971)a,c | 16.345±(6.673)b,c | 284.0±(104.6)a,b | 406.5±(165.7)a,c | 544.8±(222.4)b,c |
The primary limitation of this study lies in the inability of the chosen simulated lung to accurately replicate the airway resistance of a real airway. Furthermore, the model lung volume and compliance were fixed, and the needle was positioned vertically towards the simulated airway opening. Actual jet ventilation is influenced by a multitude of variables, including the angle and entry depth of jet needle, airway obstruction, airway resistance, lung compliance, and other physical factors. Future research needs to explore the impact of these variables, such as jet needle angle, depth, and airway obstruction, on ventilation efficiency. Further validation through animal or clinical trials is necessary.
Conclusion: In the process of jet ventilation, driving pressure, the jet needle's inner diameter, and frequency are critical determinants of minute ventilation and tidal volume. Notably, the jet needle's inner diameter, a significant variable, has frequently been underestimated in its contribution to ventilation efficacy. This element necessitates additional research to confirm its importance.
Ethical ApprovalThis investigation employs an in vitro experimental model, rendering ethical review non-applicable.
FundingThis study was supported by the Xiamen Medical and Health Guidance Project (Project Number: 3502Z20214ZD1199).
Conflict of InterestsJian-Liang Peng reports financial support, article publishing charges, and equipment, drugs, or supplies were provided by Xiamen Medical and Health Guidance Project. If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
The authors would like to express their gratitude to Chongqing Jiedingli Automation Technology Co., Ltd. for supplying equipment and offering technical support.