In 1949, Elaine Field wrote “Even with simple medical treatment the progress of most cases can be arrested, some showing considerable improvement and a few being clinically cured although the bronchograms show persistent bronchiectasis. More rarely, in mild cases the bronchographic picture over the years show regression or actual recovery in what appeared to be irreversible bronchiectasis”.1
The reversibility of radiographic bronchiectasis during an acute pulmonary infection and/or atelectasis is well known, but is radiological bronchiectasis not related to the above also reversible? For children, the answer is a clear yes (Fig. 1). Even in cystic bronchiectasis, substantial improvement can occur with treatment (see Ref. 2 in a review on paediatric bronchiectasis2). The quote above1 also depicts that the reversibility of radiologically-defined bronchiectasis in children was well known but appreciation of old knowledge sometimes gets lost until there is a resurgence in the interest in the field. This has occurred in the field of bronchiectasis, previously thought to be a rare illness, but now known to be a major contributor to respiratory morbidity worldwide.3,4
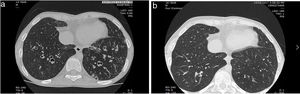
(a) Chest CT at presentation of a 13-year-old boy with a congenital heart disease depicting widespread left and right lower lobes varicose and cystic bronchiectasis. He had a chronic productive cough at presentation. (b) Chest CT of the same boy 3 years later depicting resolution of right lower lobe and many subsegments of the left lower lobe after intensive treatment including intravenous antibiotics at first diagnsosis. The adolescent was completely cough free.
Paediatric evidence-based articles have long called for early diagnosis and optimal treatment5 so as to avoid the later progressive decline in lung function and even reverse bronchiectasis in some.2 The European Respiratory Society clinical practice guidelines (ERS CPG)6 for managing children/adolescents with bronchiectasis strong (but with very low quality of evidence) recommendation include: “We recommend that where possible, interventions that prevent and/or reverse bronchiectasis are undertaken. However, these measures are context and patient specific include early identification of and treatment of inhaled foreign bodies, preventing early and severe pneumonia, preventing recurrent protracted bacterial bronchitis, treating primary immunodeficiency conditions and bronchiectasis and promoting breast feeding and immunisation”. The importance of this strong recommendation is enhanced by the fact that (i) adults with bronchiectasis who are symptomatic from childhood, compared to adult-onset disease, have worse disease and poorer prognosis (poorer lung function, more hospitalisations and worse radiological score) and (ii) a substantial proportion of adults with bronchiectasis are symptomatic from childhood (up to 80%).7
The evidence for reversibility is consistent but is low, as summarised in the ERS CPG.6 Most of the studies were retrospective, several were case reports, with a single case-control study and one prospective study.6 However, all studies showed that at least in some children/adolescents, their clinical syndrome and abnormal airway dilatation signifying radiographic bronchiectasis is reversible with appropriate management.6 The resolution or improvement rates after appropriate treatment in children with radiologically-proven bronchiectasis is as high as 63.7%8 but this proportion would invariably relate to several key factors that include the bronchiectasis severity, presence of underlying aetiology, treatment received and how bronchiectasis was defined (the diagnostic criteria used).
The concept of reversible bronchiectasis is scarce in the adult literature (other than in the atelectatic lung9). However, its importance and concept is starting to be recognised and acknowledged,9 with some adult-based respiratory physicians10,11 recognising that protracted bacterial bronchitis (PBB, a pre-bronchiectasis state) also exist in adults. Indeed, the word ‘irreversible bronchodilation’, once part of the diagnosis of bronchiectasis, is no longer in the definition of bronchiectasis for children2,6 and in some circles, also in adults.4,9
Biological mechanistic studies in bronchiectasis are lacking especially in children. Indeed, the exact mechanism of why airway dilation occurs in bronchiectasis is still debated.11 Is there a point of no return when the radiological abnormal airway dilatation can no longer be reversed? It is highly likely so, especially in adults. In post-mortem bronchiectatic specimens, bronchial dilatation is associated with loss of elastin and bronchial wall fibrosis found in less advanced specimens whilst when advanced, destruction of muscles and cartilage occurs. There are many indirect plausibility mechanistic contributors/associations. These include the following. Firstly, lung injury occurs from chronic inflammation and/or infection (factors found in bronchiectasis3), reflected also in data showing that the duration of chronic wet/productive cough is negatively correlated to lung function in non-smoking adults7 and chest CT radiological scores in children.12 Secondly, delayed bronchiectasis management is associated with poorer lung function at diagnosis but can be improved in some with optimal treatment in children.3 Thirdly, while there are similarities between children and adults, there are also substantial differences6,13; lung growth continues throughout childhood and a degree of lung repair is likely possible, with plasticity now increasingly recognised in many organs. Also, 16S rRNA studies have shown that chronic paediatric airway infections share a common core microbiota which was significant different to adults with bronchiectasis who were similar to adults with CF.14
In conclusion, paediatric data have consistently showed that the clinical syndrome with radiographic bronchiectasis is reversible. Achieving improvement and ultimately resolution is very important for their future health. We now know the deleterious effect of chronic wet cough on future lung in children12 and adults as well as future cardiac health15 and all-cause mortality.15 Achieving this requires diligent attention to chronic wet/productive cough, early diagnosis of bronchiectasis and intensive effort in optimising treatment early in the disease, including intravenous antibiotics when oral antibiotics are not effective when first diagnosed.
We clearly need novel and robust data on whether bronchiectasis may also be reversible in at least some adults and that is a challenge to adult-based physicians. We need close collaboration between paediatric and adult-based respiratory physicians so we can learn from each other so as to improve patient outcomes; thus the ERS Clinical Research Collaboration for paediatric bronchiectasis (Child-BEAR-Net [www.improveBE.org]) panel includes two internationally renowned adult-based respiratory physicians experts in bronchiectasis. Further, developing endotypes and phenotypes and/or predictive molecular tools would substantially advance this field where the disease is so heterogenous.
Conflict of InterestsABC is supported by a NHMRC Senior Practitioner Fellowship (APP1154302) and reports multiple grants from NHMRC and other fees to the institution from work relating to IDMC membership of an unlicensed vaccine (GSK), unlicensed monoclonal antibody for RSV (AZ) and a COVID-19 vaccine (Moderna) outside the submitted work. ABC also reports fees to the institution from work relating to unlicensed therapies for bronchiectasis (inhaled antibiotics from Zambon and a molecule from BI). ABC, AK and AT are leaders of Child-BEAR-Net. GR have nothing to disclose.