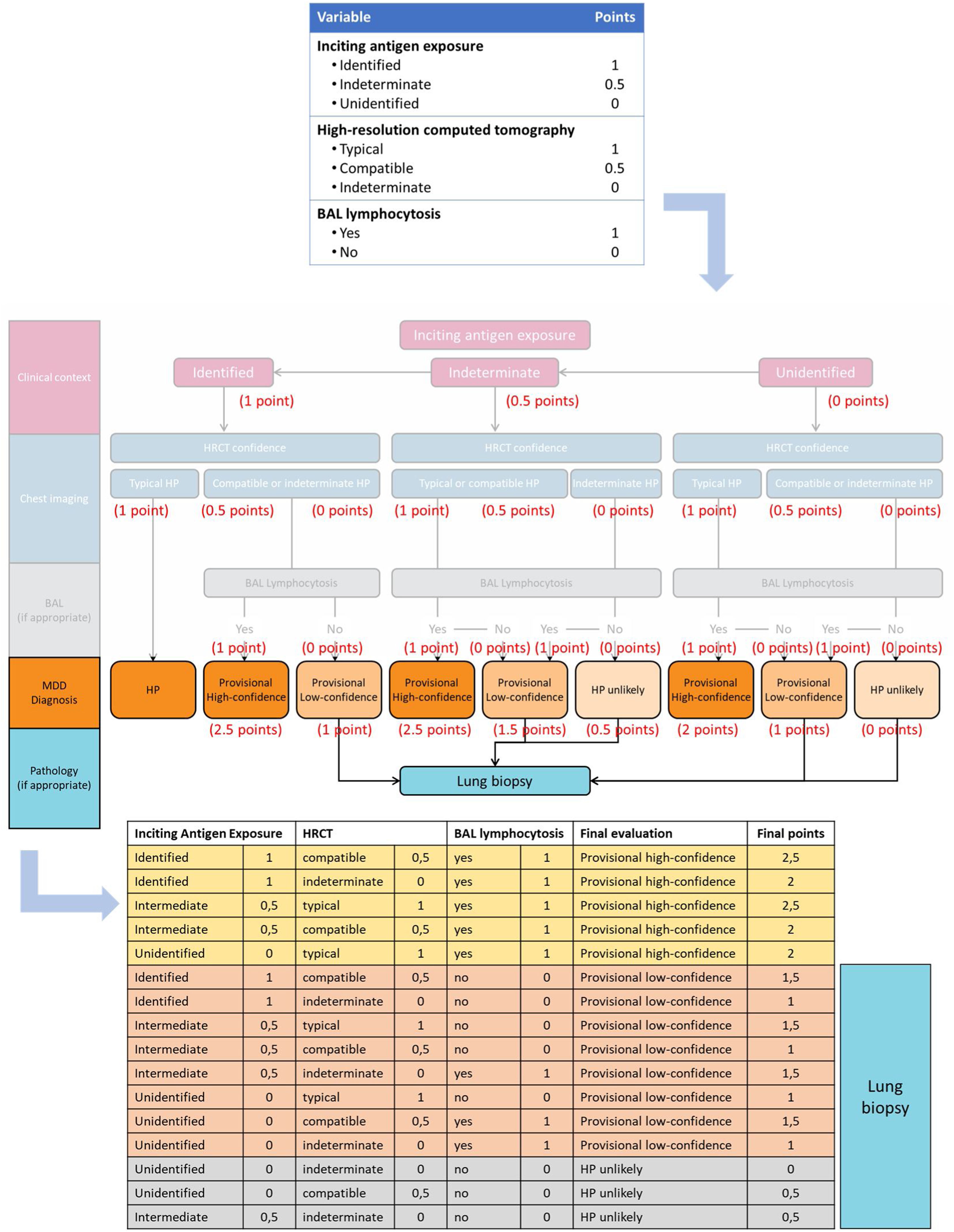
The diagnosis of interstitial lung diseases represents a current challenge for the clinician due to the low prevalence of these diseases and the consequent limited evidence for their management. Accordingly, the development of clinical recommendation documents for the management of these conditions is of special relevance for the clinician. Despite a recent document,1 a more recent new recommendation document for the diagnosis and evaluation of hypersensitivity pneumonitis (HP) have been published.2 In this new document the authors summarize the available evidence under the principles of evidence-based medicine and suggest a diagnostic algorithm (Fig. 1). This diagnostic algorithm proposes a pathway based on three main variables: exposure to an inciting antigen, high-resolution computed tomography (HRCT) findings and lymphocytosis in bronchoalveolar lavage. With these three variables the authors propose to classify cases according to the probability of having HP into high provisional probability, low provisional probability and unlikely HP. The idea behind is that those cases classified as low probability or unlikely PH would require a lung biopsy for diagnosis.
If we exclude the clinical scenario in which the patient has an exposure to a recognized inciting antigen and a typical HRCT that this establishes the diagnosis of HP, the rest of the options in the algorithm form a sufficiently complex web that may make clinical decision making difficult for the non-expert clinician. Given the visual complexity of the diagnostic algorithm, we would like to propose a quantification of each of these variables to facilitate clinical management.
Each of the three variables has different categories. As stated, exposure to an inciting antigen may be categorized as identified, indeterminate or unidentified. HRCT results are categorized into typical HP, compatible, and indeterminate findings. Finally, lymphocytosis in BAL only has two possibilities: yes or no. Thus posed, a numerical value could be given to each possibility as reflected in Fig. 1. If we apply these values to the diagnostic algorithm (Fig. 1) we can see how these scores are able to clearly separate those cases that require a lung biopsy for those cases with <2 points.
Due to the increasing knowledge of interstitial lung diseases and the complexity of radiological and histological findings, as well as the various possible clinical settings, the diagnostic approach to interstitial lung diseases is becoming progressively more complex. As a consequence, various recommendation documents have opted for a strategy of categorizing HRCT findings or tissue specimens according to the likelihood of being associated with the diagnosis under study. This strategy was first adopted for idiopathic pulmonary fibrosis3 and has been extended to the assessment of other diseases, such as HP. It is important that we make rare disease algorithms accessible to the non-expert clinician, so that we are able to apply them to daily clinical practice and thus improve the identification of these cases, improving their clinical management.