The presence of oral or naso-enteral probes during non-invasive mechanical ventilation (NIMV) increases the risk of leakage and patient discomfort. The objective of this study was to evaluate the effectiveness of a novel tube adapter for NIMV (TA-NIMV) in relation to leakage and comfort level.
MethodsA non-randomized quasi-experimental design was performed in an adult intensive care unit of a highly complex hospital, in which patients were their own controls. We included adult patients who required NIV with oronasal mask and who simultaneously had oral or naso-enteric tubes. The interventions were as follows: every participant received two therapies, one with the TA-NIMV and one conventional therapy of NIMV (CT-NIMV). Comfort could be evaluated in 99 patients with a Glasgow Coma Scale of 15. The outcomes of interest was the average percentage of air leak and patient comfort during each intervention.
Results196 patients were included in the study during a 16-month period. The mean air leak percentage was 9.2% [standard deviation (SD), 7.7] during TA-NIMV and 32.5% (SD, 12.5) during CT-NIMV (p<0.001). 84.9% reported being comfortable or very comfortable during TA-VMNI. 66.7% Uncomfortable or Very uncomfortable during CT-NIMV (p<0.001).
ConclusionHigher comfort levels and lower air leakage volume percentages were achieved using the TA-NIMV than those achieved by CT-NIMV.
La presencia de sondas orales o nasoenterales durante la ventilación mecánica no invasiva (VMNI) incrementa el riesgo de fugas y la incomodidad del paciente. El objetivo de este estudio fue evaluar la efectividad de un novedoso adaptador de sondas para VMNI (AS-VMNI) en relación con las fugas y nivel de comodidad.
MétodosSe realizó un diseño cuasiexperimental no aleatorizado en la unidad de cuidados intensivos del adulto de un hospital de alta complejidad, en el cual los pacientes fueron sus propios controles. Se incluyeron pacientes adultos que requerían VMNI con máscara oronasal y que tenían simultáneamente sondas orales o nasoenterales. Cada participante recibió 2 tratamientos: uno con el AS-VMNI y otro, convencional, con VMNI (CT-NIMV). La comodidad pudo evaluarse en 99 pacientes con un 15 en la escala de coma de Glasgow. Las variables de resultado fueron el porcentaje de fugas y la comodidad del paciente durante cada una de las intervenciones.
ResultadosCiento noventa y seis pacientes fueron incluidos en el estudio durante un período de 16 meses. El porcentaje medio de fuga de aire fue del 9,2% (desviación estándar, 7,7) durante el AS-VMNI y del 32,5% (desviación estándar, 12,5) durante el TC-VMNI (p<0,001). El 84,9% de los pacientes refirieron sentirse cómodos o muy cómodos durante AS-VMNI. El 66,7% refirieron estar incómodos o muy incómodos durante TC-NIMV (p<0,001).
ConclusiónEl uso del AS-VMNI permitió mayores niveles de comodidad y menores porcentajes de fugas de aire que con el TC-VMNI.
Non-invasive mechanical ventilation (NIMV) is an accepted supportive strategy widely used in patients with acute respiratory failure from both hypercapnic and hypoxemic origin.1–4 NIMV can also prevent re-intubation in some cases and might provide comfort at the end of life.5,6 Nevertheless, NIMV can fail because many factors including inappropriate selection of individual cases and patient–ventilator asynchrony.7 Conversely to invasive mechanical ventilation, NIMV is characterized by an open and non-hermetic circuit that is intrinsically leaky. These air leaks pose a challenge for respiratory support because they create a mismatch between the flow provided by the ventilator and the flow effectively delivered to the patient, leading sometimes to considerable asynchrony, discomfort, and ultimately, to fail of NIMV support.
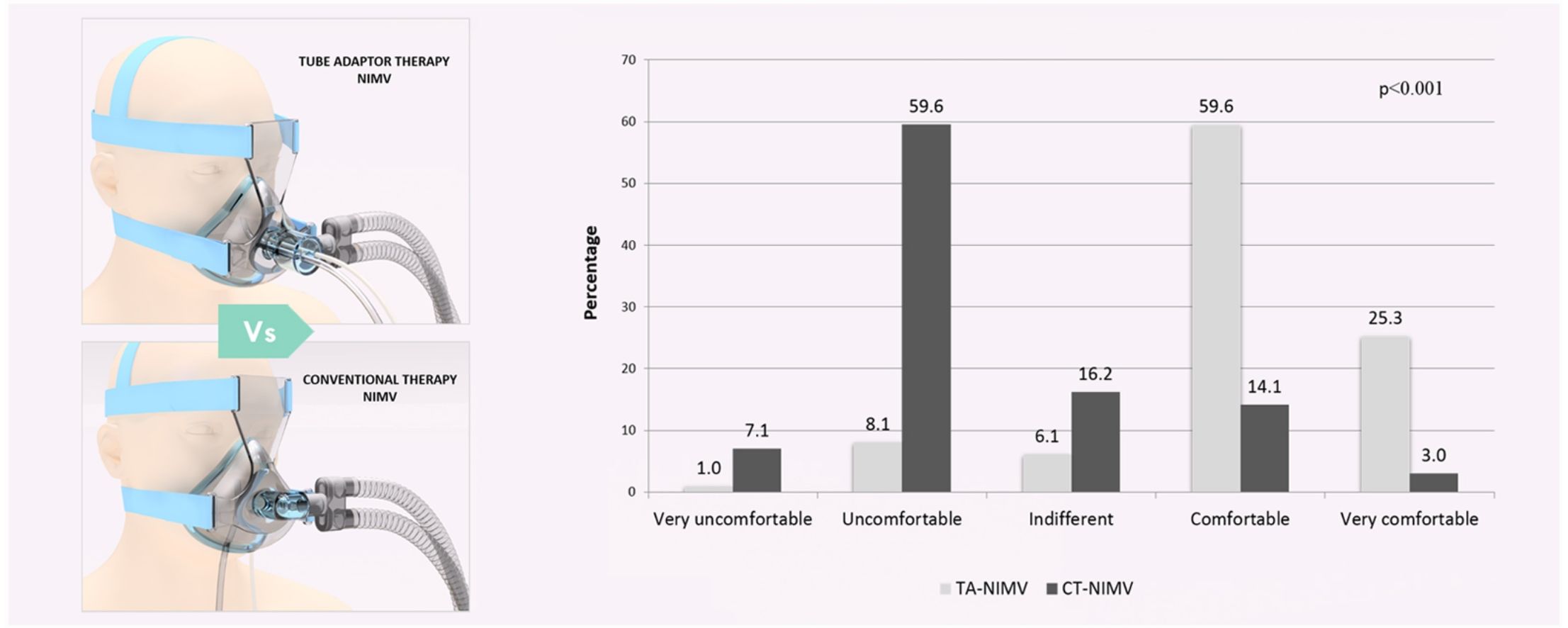
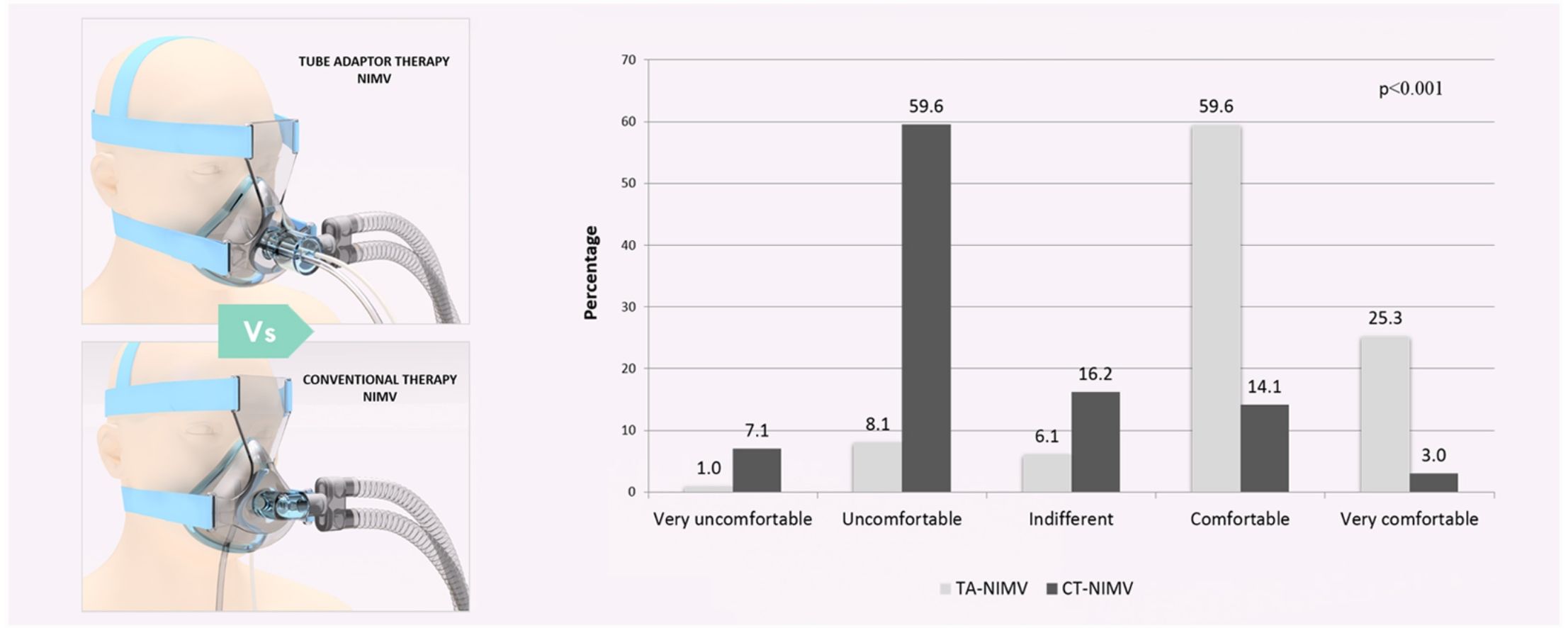
Critically ill patients often require enteral tubes to provide nutritional support or administering medications.8–11 These tubes can increase the risk of air leaks when NIMV is provided through oro-nasal interfaces.12,13 Although air leaks can be clinically challenging, their magnitude might sometimes be reduced by adjusting the patient interface but it can increase the patient's discomfort and cause skin lesions.15 Similarly, specific algorithms for leak compensation have been incorporated into the latest generation of ventilators to reduce these adverse effects with non consistent clinical results.14 Thus, we develop a new tube adaptor for NIMV (TA-NIMV) designed to minimize air leaks by improving the adjust of the oro-nasal interfaces in patients in whom an enteral tube has been placed. In this first report, we evaluate the impact of such TA-NIMV on the reduction of air leaks and the subjective comfort perceived by the patient during NIMV support.
Materials and methodsStudy designA non-randomised, clinical intervention (quasi-experimental design) was conducted in a 90-bed mixed intensive care unit during a sixteen-month period. Patients with one or more naso-enteric or oro-enteric tube(s) in place and requiring NIMV support through an oro-nasal mask interface were included in the study. Then, they received in a random order a run of at least 60min of NIVM using the tube adaptor (TA-NIMV) or the conventional therapy (CT-NIMV). The percentage of air leaks and patients comfort was registered after a stabilization period of at least 15min in each run. A “washout period” of at least 4h between each VMNI run was ensured to avoid potential interferences between TA-NIMV and CT-NIMV strategies.
ParticipantsAll adult patients (≥18 years old) admitted to the ICU by any cause, requiring NIMV support thorough an oro-nasal interface and simultaneously requiring a naso-enteric tube in place for nutrition, enteral decompression, or drug administration. NIMV was performed following the institutional protocol and international guidelines.16,17 Patients were excluded if they had any contraindication for NIMV use. The absolute contraindications were respiratory arrest, uncontrolled vomiting, or massive upper gastrointestinal bleeding, upper airway obstruction, facial trauma, pregnancy and refusal to participate (not willing to sign the consent form). The relative contraindications were hypotensive shock, uncontrolled cardiac ischaemia or arrhythmia, agitation, being uncooperative, inability to protect the airway due to swallowing impairment, excessive secretions (not possible to manage by clearance techniques), multiple organ failure, recent upper airway or upper gastrointestinal surgery and progressive severe respiratory failure. In addition, patients with pulmonary bullae, bronchopleural fistula, or persistent pneumothorax were excluded from the study.
InterventionsEach eligible participant received NIMV support alternatively using the TA-NIMV and another therapy without the tube adaptor (CT-NIMV). Therefore, the patients were their own controls. Blinding and masking were not feasible because the tube adaptor was visible during the NIMV therapies and the evaluations for air leak and patient comfort were deemed performed at bedside.
Assignment methodNIMV therapy was performed according to individual needs. NIMV was usually given for periods of at least 60min according to the attending recommendation. NIMV was alternatively started by using the tube adaptor (TA-NIMV) or the conventional NIMV support (CT-NIMV), followed by the other strategy during the next NIMV run, after a washout period of at least 4h. This method was sequentially performed until the desired sample size was reached. The ventilator parameters were maintained throughout the two interventions. These paired interventions were performed once in each patient. General ICU management was continued for each patient following institutional protocols.
The NIMV oro-nasal masks (RESMED®) were classified by size in accordance with each patient's facial morphology. The ventilator used was either SERVO-i® or SERVO-s®. Ventilator leakage was defined as the amount of ICV lost and was recorded in terms of percentage.
Adaptor designThe size of the enteric tube was fundamental to developing the tube adaptor for this study. There were two types of enteric tubes used in our adult ICU patients. The gastric drainage probe (Levin, Salem, Miller Abbott), which was used to administer medications and control gastric contents, had varying sizes that ranged from 14F (4.0mm) to 20F (7.3mm), with an outer diameter of approximately 9mm on its distal end. The tube for enteral feeding was usually of the 12F (4.0mm) caliber and had a universal two-way connector that measured approximately 17-mm wide on its distal end; it was used for nutritional support and administration of medications or fluids.
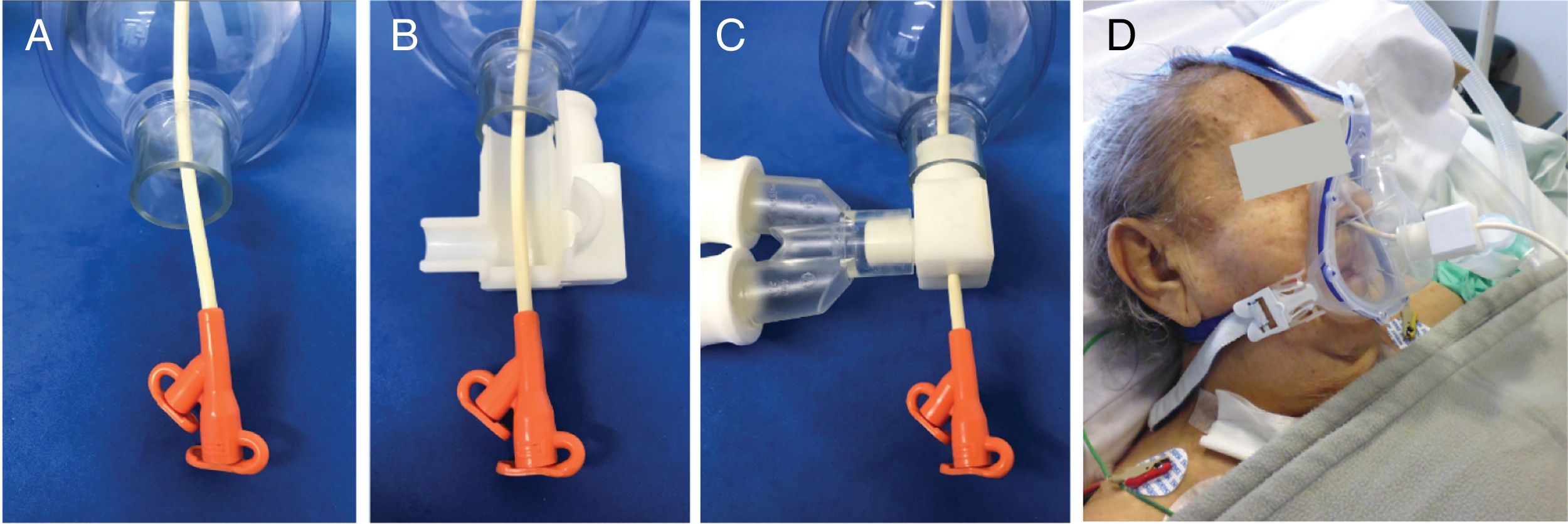
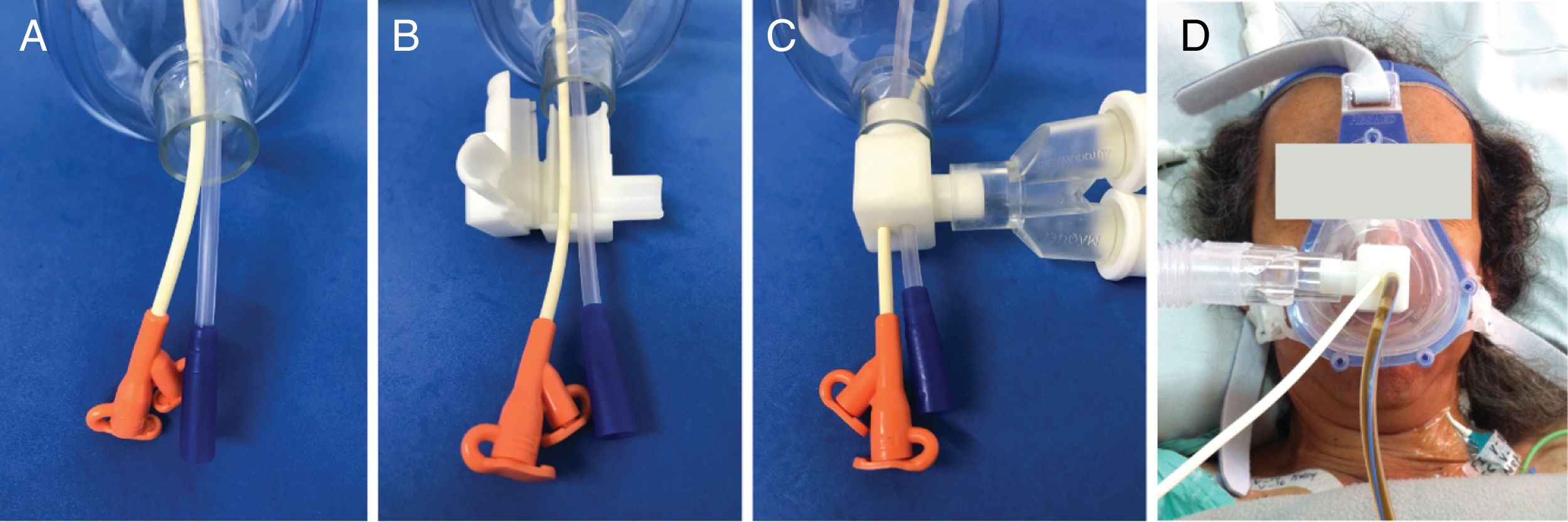
The tube adaptor device was made of a rigid polymer plastic for one or two enteric tubes sizes. The adapter that interfaces between ventilator circuit and mask opens laterally, allowing tubes passing through the center of the mask to be placed in appropriately sized holes, when closed, it is inserted in the mask and attached to ventilator in patients whit one (Fig. 1) or two (Fig. 2) enteric tubes.
Therapeutic use of tube adaptor for NIMV with one tube. (A) The tube for enteral feeding is passed through the central hole of the mask. (B) The tube adaptor for non-invasive mechanical ventilation is opened. (C) The tube adaptor for non-invasive mechanical ventilation closed around the tube, inserted in the mask and attached to the ventilator circuit. (D) The use of a tube adaptor for one tube for enteral feeding during non-invasive mechanical ventilation therapy in a representative patient.
Therapeutic use of tube adaptor for NIMV with two tubes. (A) The tube for enteral feeding and gastric drainage probe are passed through the central hole of the mask. (B) The tube adaptor for non-invasive mechanical ventilation is opened. (C) The tube adaptor for non-invasive mechanical ventilation closed around the tubes, inserted into the mask and attached to ventilator circuit. (D) The use of a tube adaptor for tube for enteral feeding and gastric drainage probe during non-invasive mechanical ventilation therapy in a patient.
The demographics (e.g. age and sex) and clinical information (i.e. reasons for NIMV) were obtained from the FVL electronic medical charts. Clinical examinations provided information on the use of dental prosthesis and the presence of abundant beard. Naso-enteric tubes (Nutritional Jejune) are classified according to calibre and usage, but the usual standard is 12F; in our patients, the sizes of the gastric tubes were 14F, 16F, 18F and 20F.
The respiratory parameters were obtained from the ventilator, and the hemodynamic parameters were obtained from the central monitor. The average of six recordings were calculated for the following parameters: heart rate, blood pressure, oxygen saturation (SO2), fraction of inspired oxygen (FiO2), inspiratory tidal volume (ITV), expiratory tidal volume (ETV), respiratory rate and percentage of air leak. Ventilator mode and positive-end expiratory pressure (PEEP) were also recorded.
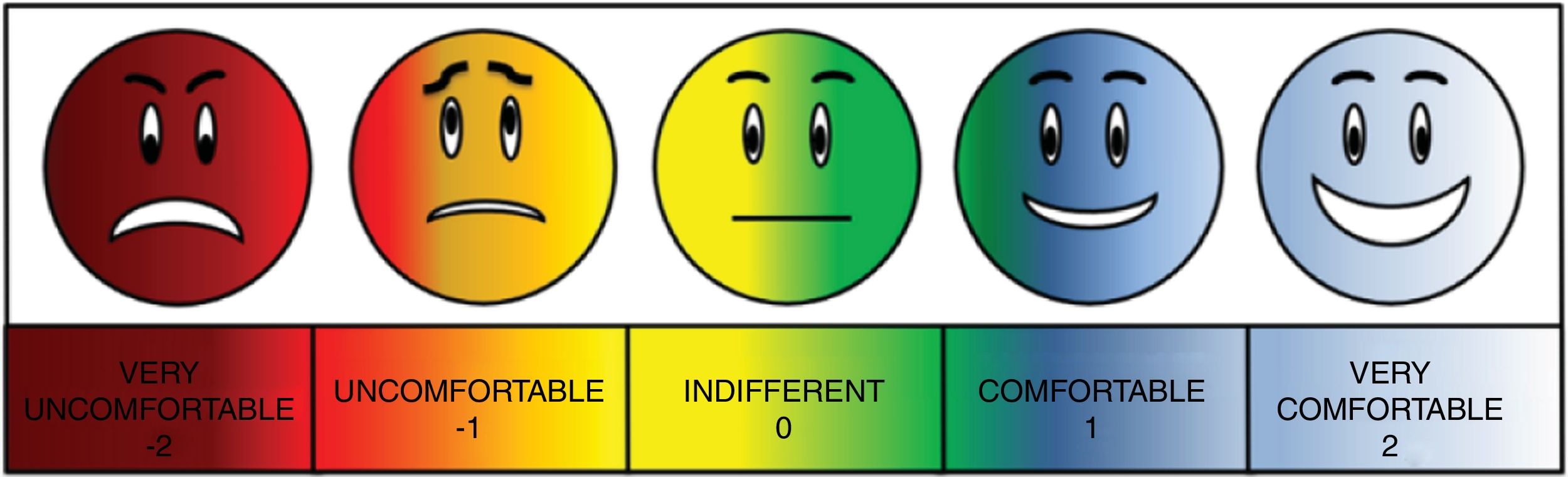
The main outcomes were the average percentage of air leak and patient comfort during each intervention. To assess comfort, a visual analogue scale of comfort (VASC) was developed. A preliminary version of the VASC was tested on patients with no neurologic involvement, and its use was then explored using techniques according to the types of cognitive procedures, such as thinking aloud, verbal tests and ethnography.18
A focal group of physicians, all of whom were experienced in management and use of scales, developed the final version of the scale, which included the use of colours (Fig. 3). The VASC was classified as −2=very uncomfortable, −1=uncomfortable, 0=indifferent, 1=comfortable and 2=very comfortable. It was applied only to patients with Glasgow coma scale (GCS) of 15 (n=99) at the time of bedside data collection during each intervention.
The variables were collected by ICU therapists onto a standardised paper format, designed for the purpose of this study, then were entered into an electronic database. The data on respiratory and hemodynamic parameters were collected 15min after each intervention, whereas the data on comfort were obtained at the end of each intervention.
Sample sizeThe outcome of interest for sample size calculation was the air leak percentage. To our knowledge, there had been no studies evaluating the effectiveness of devices for two enteric tubes in patients requiring NIMV with oro-nasal interface. A literature review of studies that evaluated the devices’ effectiveness for one enteric tube in patients requiring NIMV with an oro-nasal interface revealed that the air leak percentage ranged between 25% and 60%.19,20 We expected an average of 30% air leaks during CT-NIMV. We assumed that an air leak percentage up to 21% would be clinically significant and tolerable for an acceptable NIMV therapy. Therefore, with a power of 80% and a significance of 5%, the estimated sample size for one-sample comparison of proportions was 191 patients. With this sample size, a 9% absolute reduction in air leak was supposed to be observed during TA-NIMV.
Statistical analysesQualitative variables were presented as absolute and relative frequencies. They were presented as mean with standard deviation (SD) or as median with 25th and 75th interquartile range (IQR). Comparisons of quantitative variables between the two interventions were performed using paired Student's t-test or Wilcoxon matched pairs test, as appropriate. Patient comfort on the VASC was compared between interventions using the marginal homogeneity test (Stuart–Maxwell). The main outcomes were compared between TA-NIMV and CT-NIMV using paired χ2 test. Subgroup analyses were performed based on the number and sizes of enteral tubes. p values <0.05 were considered statistically significant. All analyses were performed using Stata (version 12.1) software.
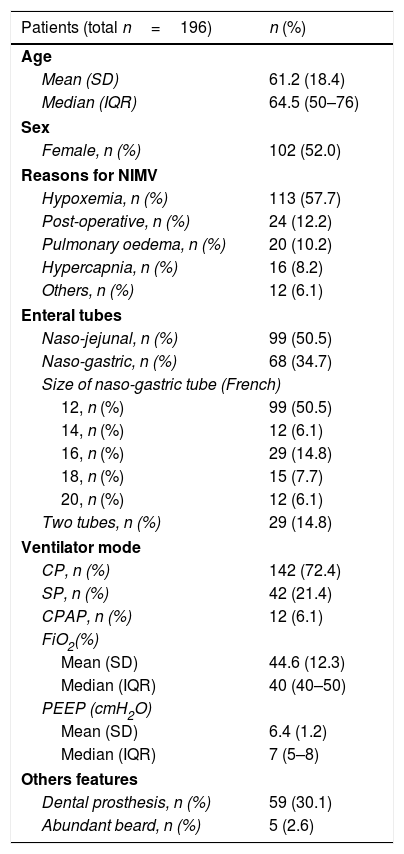
ResultsThere were 196 patients studied between October 2012 and January 2014. The mean age was 61.2 years (SD, 18.4 years) and 102 (52.0%) were women. The reasons for NIMV were hypoxemia in 113 patients (57.7%), post-operative respiratory distress in 24 (12.2%), pulmonary oedema in 20 (10.2%), hypercapnia in 16 (8.2%) and others in 12 (6.1%). Ninety-nine patients (50.5%) had a naso-enteric tube and 68 (34.7%) a naso-enteric tube. The size of the naso-enteric tube was 12F in 99 patients (50.5%), 14F in 12 (6.1%), 16F in 29 (14.8%), 18F in 15 (7.7%) and 20F in 12 (6.1%). There were 29 patients (14.8%) who required simultaneous use of more than one naso-enteric tube.
The mean washout period between the two interventions was 5.48h (SD, 2.94h). The ventilator mode was control pressure in 142 patients (72.4%), support pressure in 42 (21.4%) and continuous positive airway pressure in 12 (6.1%). The mean FiO2 was 44.6% (SD, 12.3%), and the median PEEP was 7 (IQR, 5–8). Dental prostheses were used in 59 patients (30.1%), and abundant beard was noticed in five patients (2.6%) (Table 1).
Baseline characteristics of the participants.
| Patients (total n=196) | n (%) |
|---|---|
| Age | |
| Mean (SD) | 61.2 (18.4) |
| Median (IQR) | 64.5 (50–76) |
| Sex | |
| Female, n (%) | 102 (52.0) |
| Reasons for NIMV | |
| Hypoxemia, n (%) | 113 (57.7) |
| Post-operative, n (%) | 24 (12.2) |
| Pulmonary oedema, n (%) | 20 (10.2) |
| Hypercapnia, n (%) | 16 (8.2) |
| Others, n (%) | 12 (6.1) |
| Enteral tubes | |
| Naso-jejunal, n (%) | 99 (50.5) |
| Naso-gastric, n (%) | 68 (34.7) |
| Size of naso-gastric tube (French) | |
| 12, n (%) | 99 (50.5) |
| 14, n (%) | 12 (6.1) |
| 16, n (%) | 29 (14.8) |
| 18, n (%) | 15 (7.7) |
| 20, n (%) | 12 (6.1) |
| Two tubes, n (%) | 29 (14.8) |
| Ventilator mode | |
| CP, n (%) | 142 (72.4) |
| SP, n (%) | 42 (21.4) |
| CPAP, n (%) | 12 (6.1) |
| FiO2(%) | |
| Mean (SD) | 44.6 (12.3) |
| Median (IQR) | 40 (40–50) |
| PEEP (cmH2O) | |
| Mean (SD) | 6.4 (1.2) |
| Median (IQR) | 7 (5–8) |
| Others features | |
| Dental prosthesis, n (%) | 59 (30.1) |
| Abundant beard, n (%) | 5 (2.6) |
SD, standard deviation; IQR, interquartile range; NIMV, non-invasive mechanical ventilation; CP, control pressure; SP, support pressure; CPAP, continuous positive airway pressure; FiO2, fraction of inspired oxygen; PEEP, positive-end expiratory pressure.
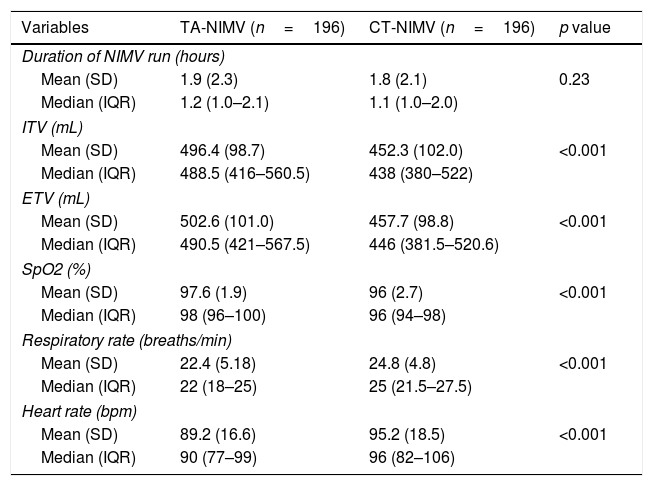
Comparisons of the respiratory and hemodynamic parameters between interventions are presented in Table 2. The mean duration was similar (p=0.23) between the TA-NIMV [1.96h (SD, 2.33h)] and the CT-NIMV [1.8h (SD, 2.13h)]. Compared with the CT-NIMV group, the TA-NIMV group had significantly higher mean ITV [496.4 (SD, 98.7) vs. 452.3 (SD, 102.0); p<0.001]; mean ETV [502.6 (SD 101.0) vs. 457.7 (SD, 98.8); p<0.001)] and mean SO2 [97.6% (SD, 1.9%) vs. 96.0% (SD, 2.7%); p<0.001)]. The mean respiratory rate and heart rate were significantly lower in the TA-NIMV group than in the CT-NIMV group (Table 2).
Respiratory and hemodynamic parameters during non-invasive mechanical ventilation.
| Variables | TA-NIMV (n=196) | CT-NIMV (n=196) | p value |
|---|---|---|---|
| Duration of NIMV run (hours) | |||
| Mean (SD) | 1.9 (2.3) | 1.8 (2.1) | 0.23 |
| Median (IQR) | 1.2 (1.0–2.1) | 1.1 (1.0–2.0) | |
| ITV (mL) | |||
| Mean (SD) | 496.4 (98.7) | 452.3 (102.0) | <0.001 |
| Median (IQR) | 488.5 (416–560.5) | 438 (380–522) | |
| ETV (mL) | |||
| Mean (SD) | 502.6 (101.0) | 457.7 (98.8) | <0.001 |
| Median (IQR) | 490.5 (421–567.5) | 446 (381.5–520.6) | |
| SpO2 (%) | |||
| Mean (SD) | 97.6 (1.9) | 96 (2.7) | <0.001 |
| Median (IQR) | 98 (96–100) | 96 (94–98) | |
| Respiratory rate (breaths/min) | |||
| Mean (SD) | 22.4 (5.18) | 24.8 (4.8) | <0.001 |
| Median (IQR) | 22 (18–25) | 25 (21.5–27.5) | |
| Heart rate (bpm) | |||
| Mean (SD) | 89.2 (16.6) | 95.2 (18.5) | <0.001 |
| Median (IQR) | 90 (77–99) | 96 (82–106) | |
TA-NIMV, non-invasive mechanical ventilation with tube adaptor; CT-NIMV, non-invasive mechanical ventilation without tube adaptor (conventional therapy); SD, standard deviation; IQR, interquartile range; ITV, inspiratory tidal volume; ETV, expiratory tidal volume; SO2, oxygen saturation.
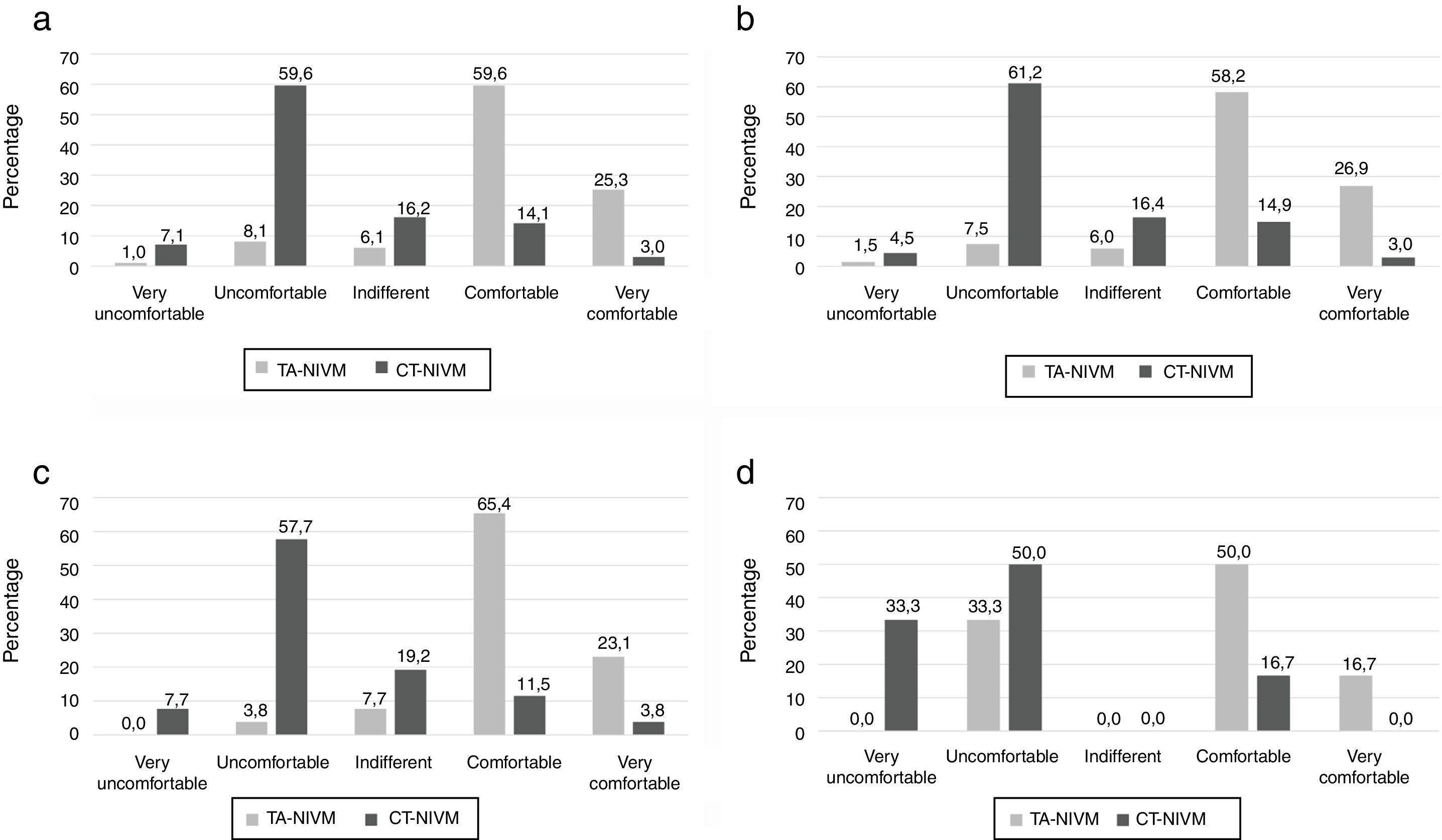
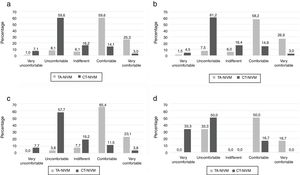
Evaluating comfort after the intervention was possible in 99 patients with a GCS of 15. After TA-NIMV 59 patients (59.6%) reported being comfortable, and 25 patients (25.3%) reported being very comfortable. After CT-NIMV, 14 patients (14.1%) reported being comfortable, while only three patients (3.0%) reported being very comfortable. The use of TA-NIMV was significantly more comfortable than CT-NIMV when PCV or PSV modes were used (Fig. 4).
Comparisons comfort between interventions. (a) Percentage of comfort perception during TA-NIMV and CT-NIMV in all patients evaluated (n=99), p<0.001. (b) Percentage of comfort among patients on pressure support mode, (n=67), p<0.001. (c) Percentage of comfort among patients on pressure control mode, (n=26), p<0.001. (d) Percentage of comfort among patients on continuous positive airway pressure ventilation mode, (n=6), p<0.261. Differences between groups were tested using the marginal homogeneity test (Stuart–Maxwell).
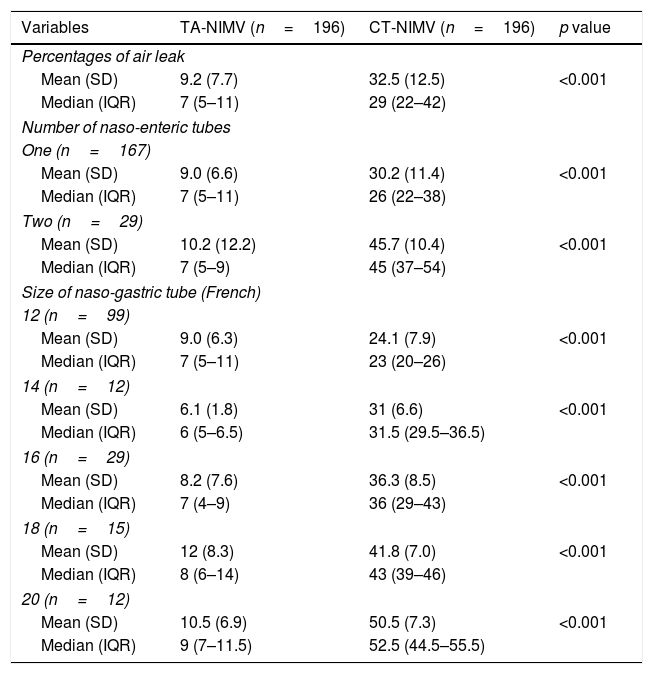
In all patients (n=196), the mean air leak percentage was 9.2% (SD, 7.7%) during TA-NIMV and 32.5% (SD, 12.5%) during CT-NIMV (p<0.001). Subgroup analyses by the numbers and sizes of naso-enteric tubes showed that the air leak percentages were significantly lower with TA-NIMV than with CT-NIMV (Table 3).
Comparison of the percentages of air leak between the types of interventions, stratified by the number and size of enteric tubes.
| Variables | TA-NIMV (n=196) | CT-NIMV (n=196) | p value |
|---|---|---|---|
| Percentages of air leak | |||
| Mean (SD) | 9.2 (7.7) | 32.5 (12.5) | <0.001 |
| Median (IQR) | 7 (5–11) | 29 (22–42) | |
| Number of naso-enteric tubes | |||
| One (n=167) | |||
| Mean (SD) | 9.0 (6.6) | 30.2 (11.4) | <0.001 |
| Median (IQR) | 7 (5–11) | 26 (22–38) | |
| Two (n=29) | |||
| Mean (SD) | 10.2 (12.2) | 45.7 (10.4) | <0.001 |
| Median (IQR) | 7 (5–9) | 45 (37–54) | |
| Size of naso-gastric tube (French) | |||
| 12 (n=99) | |||
| Mean (SD) | 9.0 (6.3) | 24.1 (7.9) | <0.001 |
| Median (IQR) | 7 (5–11) | 23 (20–26) | |
| 14 (n=12) | |||
| Mean (SD) | 6.1 (1.8) | 31 (6.6) | <0.001 |
| Median (IQR) | 6 (5–6.5) | 31.5 (29.5–36.5) | |
| 16 (n=29) | |||
| Mean (SD) | 8.2 (7.6) | 36.3 (8.5) | <0.001 |
| Median (IQR) | 7 (4–9) | 36 (29–43) | |
| 18 (n=15) | |||
| Mean (SD) | 12 (8.3) | 41.8 (7.0) | <0.001 |
| Median (IQR) | 8 (6–14) | 43 (39–46) | |
| 20 (n=12) | |||
| Mean (SD) | 10.5 (6.9) | 50.5 (7.3) | <0.001 |
| Median (IQR) | 9 (7–11.5) | 52.5 (44.5–55.5) | |
TA-NIMV, non-invasive mechanical ventilation with tube adaptor; CT-NIMV, non-invasive mechanical ventilation without tube adaptor (conventional therapy); SD, standard deviation; IQR, interquartile range.
In this study, we presented the feasibility and actual effectiveness of a device designed by our hospital ICU staff. Our results suggested that using the new tube adaptor for NIMV administered, via an oro-nasal mask in patients with one or two naso-enteral tubes, improved patient comfort and significantly decreased the air leakage volume. The statistically significant lower sir leak percentages with TA-NIMV than with CT-NIMV were consistent among all subgroup analyses.
NIMV had been shown to significantly decrease mortality,21 but the factors that determine its success are based on adequate tolerance and the patient's comfort. Previously conducted studies have proved that the magnitude of air leaks is correlated with the number of ineffective breaths and severity of delayed cycling, both of which play important roles in generating patient–ventilator asynchrony and discomfort.19 We designed our device aiming to decrease air leaks to improve patient comfort. Moreover, we observed that patients who were placed on TA-NIMV had higher comfort levels than those who were not placed on TA-NIMV. Our device possibly had beneficial effects even though we did not measure patient–ventilator asynchrony metrics.
Significant air leaks can induce a pressure drop or generate flows that are perceived as patient inspiratory effort. These inevitably results in auto-triggering, which is a highly undesirable phenomenon that can be resolved only by reducing triggering sensitivity. This reduction in triggering sensitivity reportedly leads to late cycling or failure to trigger in 12%–23% of patients.19
When a tube adaptor was added to the NIMV, approximately 85% of patients with GCS of 15/15 confirmed that they felt comfortable or very comfortable. By utilising a special mask that engaged the naso-enteric tubes based on a scale of 1 to 5, our results were consistent with those obtained by Gregoretti et al.,22 who reported significant improvement with respect to patient comfort levels.
We described the effects of a new device that decreased air leak in cases treated with NIMV via an oro-nasal mask with concomitant use of one or two naso-enteric tubes. These findings were consistent regardless of the number and size of the naso-enteric tubes. Few articles have reported using tube adaptors in NIMV.22 Moreover, much less is known about the comparative effectiveness between a mask prototype with a port for the naso-enteric tube and a conventional mask. A case report demonstrated that using a special endoscopy mask with a 16F probe for the enteral tubes reduced the risks of failure and improved NIMV quality in two patients.23 At the moment, there had been no reports on using NIMV oro-nasal mask in patients who needed more than one enteric tube.
Our results showed using the tube adaptor maintained the air leak percentage below 10%, except in the subgroup of patients with 20F enteric tubes; in that group, the air leak percentage reached slightly above 10%. Nevertheless, the differences between TA-NIMV and CT-NIMV were statistically significant, and the air leak percentage was much higher with CT-NIMV. Reducing the air leak percentage with our new device may improve the outcomes of critically ill patients who usually require multiple interventions.
Current ventilators can be programmed to deliver between 40L/min and 65L/min to compensate for air leaks.24 However, excessive air leaks cannot be well compensated, and the use of NIMV becomes ineffective when air leaks exceed 20%.25,26 In particular, this is an important finding for institutions in low- to middle-income countries, which rarely have such technology.
LimitationsThis study had some limitations and the results should be interpreted in the context of the patients included. We did not actively evaluate some adverse effects related to oro/naso mask interface such a skin irritation or abrasions. Nevertheless, all patients received skin protection barriers according to the local protocol. Further bias could have been introduced because the outcome evaluators were not blinded to the interventions. However, the comparisons were performed in the same patients as their own controls. Therefore, the addition of a tube adaptor seems to reduce air leaks and improve patient comfort compared to those during conventional NIMV.
ConclusionThe use of a tube adaptor to adjust NIMV mask interfaces in patients in whom oro- or naso-enteral tubes are in place, significantly reduces air leaks and improves subjective comfort perceived by the patient during NIMV support.
AuthorshipOscar I. Quintero: Conception and design of the study, writing the core content of the study, analysis and interpretation of data, drafting the article or revising it critically for important intellectual content.
Alvaro I. Sanchez: Writing the core content of the study, coordinated delivery of interventions, analysis and interpretation of data, preparation and critical review of the manuscript.
Paola A. Chavarro: Writing the core content of the study, coordinated delivery of interventions, analysis and interpretation of data, preparation and critical review of the manuscript.
Isabel C. Casas: Writing the core content of the study, analysis and interpretation of data, preparation and critical review of the manuscript.
Gustavo A. Ospina Tascón: Writing the core content of the study, coordinated delivery of interventions, analysis and interpretation of data, preparation and critical review of the manuscript.
All authors declare their approval for the current version of the manuscript.
FundingThis work was funded by Fundación Valle del Lili (Centro de Investigaciones Clínicas), Grand 00576/12.
Conflict of interestThe authors declare one conflict of interest. Fundación Valle del Lili has the device patent of the tube adapter for non-invasive mechanical ventilation. The patent number 1165 is registered at the Colombian Patent and Trademark Office (Superintendencia de Industria y Comercio de la Republica de Colombia). International publication is WO2014188242A1 of World Intellectual Property Organization.
This study was supported by Fundación Valle del Lili (Centro de Investigaciones Clínicas). The authors would like express their gratitude towards ICU Physiotherapists who helped in the collection of study data. We also extend our thanks to Dr. Alejandro Castillo Martinez and other members of the medical group of the Department of Psychiatry of the Fundación Valle del Lili for their support in the development of the Visual Analogue Scale of Comfort.