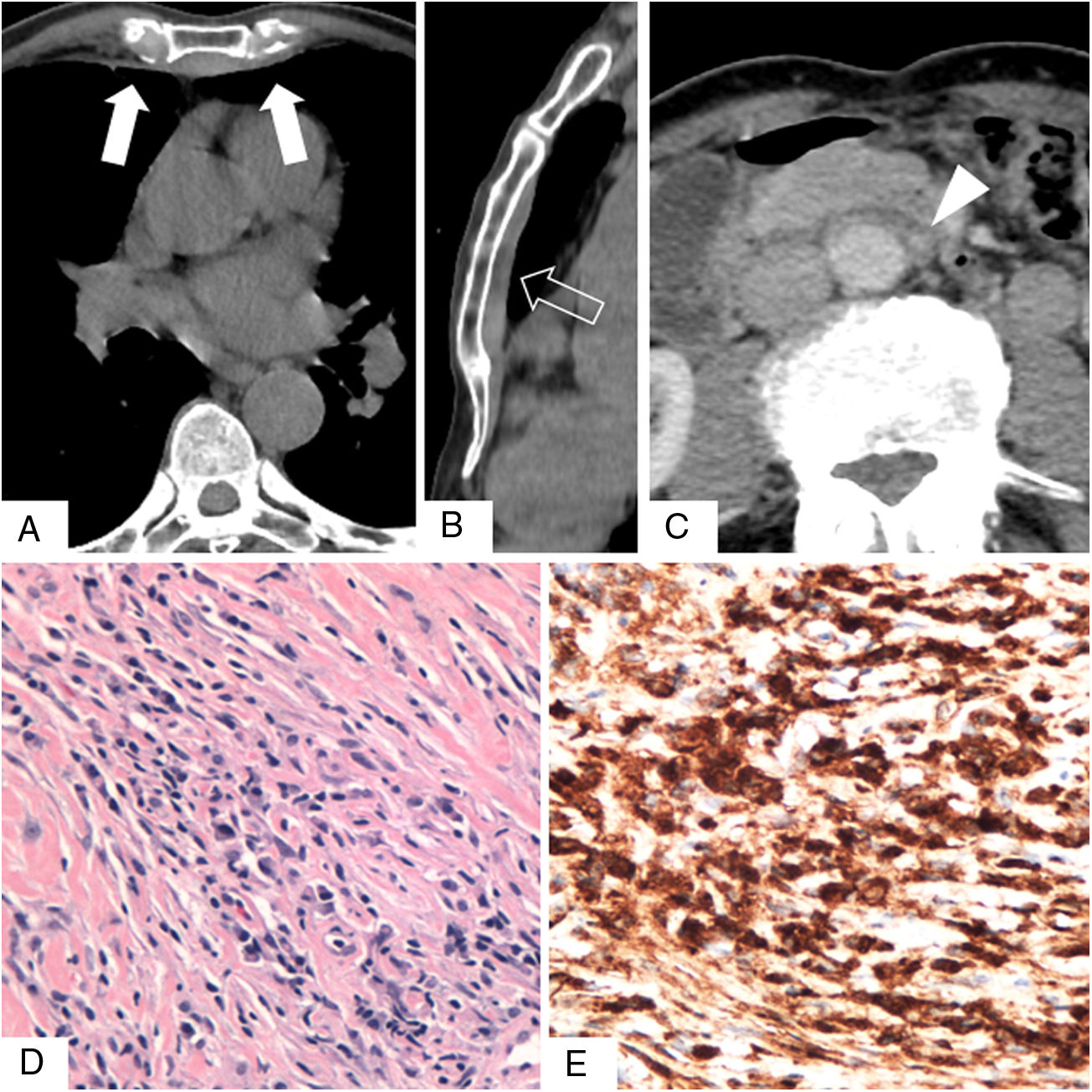
We report the case of a 78-year-old man with a previous history of asbestos exposure for 13 years, who presented with dyspnea. The patient packed asbestos-containing waste materials until the age of 50. Thus, the latency period was 28 years. Chest computed tomography showed an irregular, uncalcified pleural plaque in the anterior right hemithorax. One year later, the plaque had flattened, extending axially to the retrosternal mediastinum and contralateral pleural space (Fig. 1A and B). A small soft-tissue mass surrounding the abdominal infrarenal aorta was also identified (Fig. 1C). Transthoracic percutaneous biopsy revealed storiform fibrosis with polyclonal lymphoplasmocytic and plasma cell infiltration. Additionally, immunoglobulin G4 (IgG4) expression was found in plasma cells, with an IgG4/IgG ratio >50% (Fig. 1D and E). The serial IgG4 concentration was found to be high (5920mg/L), and a final diagnosis of IgG4-related bridging pleural fibrosis (BPF) with retrosternal fibrosclerosis (RF) was established.
Unenhanced chest computed tomography scans obtained in the axial plane (A) and with sagittal reformatting (B), showing a flat, uncalcified anterior pleural plaque “bridging” the hemithoraces (arrows in A, open arrow in B). (C) Axial contrast-enhanced abdominal scan showing the periaortic soft tissue mass (arrowhead). (D) Photomicrograph of the pleural plaque showing storiform fibrosis and lymphoplasmacytic infiltrate (hematoxylin-eosin stain). (E) Immunohistochemical staining showing immunoglobulin G4 positivity in plasma cells.
BPF refers to continuous bilateral anterior pleural thickening that “bridges” the hemithoraces and involves the retrosternal area, resulting in RF.1,2 BPF and RF have been described in association with retroperitoneal fibrosis, and in the patient described here a subtle retroperitoneal soft-tissue mass surrounding the infrarenal aorta was also observed. These patterns have been described in asbestos-exposed patients and in those with immunoglobulin G4-related sclerosing disease (IgG4SD).1–4
Asbestos-related pleural fibrosis usually appears as bilateral, partially calcified plaques involving the parietal pleura, and is quite different from the pleural thickening observed in our patient.1,5 Uibu et al.4 studied pleuro-pulmonary manifestations in a series of 48 asbestos-exposed patients with RF and found atypical pleural plaques extending to the anterior mediastinum in three patients, recognizing such plaques as rare findings and speculating that asbestos may lead to severe fibrotic changes in some susceptible individuals.
Imaging findings for mediastinal fibrosis were also atypical in this case; the characteristic features of this entity are an often-calcified invasive mass in the middle mediastinal compartment, encasing vascular and bronchial structures. In the case described here, we observed a different pattern of isolated, uncalcified retrosternal fibrosis.1
IgG4SD is a multisystem clinical-pathological entity described in the last decade, characterized by fibro-inflammatory lesions rich in IgG4-positive plasma cells.6 Thoracic involvement may occur in several patterns, comprising pulmonary lesions (nodules, ground-glass opacities, alveolar-interstitial disease and bronchovascular disease), pleural thickening and mediastinal lesions (mediastinal fibrosis and lymphadenopathy).6,7 Two sets of diagnostic criteria have been proposed: the Japanese criteria, which involve clinical, serological IgG4 levels and histopathological features of the disease, and the Boston criteria, which are histopathological.8,9 Recently, the Japanese team updated and proposed an organ-specific approach.10
Some authors have speculated about a possible association between asbestos exposure and IgG4SD, arguing that the latter may arise due to hypersensitivity of the regulatory immune system to atopic conditions induced by asbestos.3,11 IgG4SD shares some characteristics with allergic disorders, such as elevated T helper 2 (Th2) cell, regulatory cytokine and serum immunoglobulin E (IgE) levels; additionally, mast cells in IgG4SD show strong positivity for IgE.12 Thus, IgG4SD has been considered to be a potentially allergic condition, and asbestos could be the trigger inducing persistent Th2 responses and mast cell activation by sustained IgE production.12 The literature contains some case reports and case series describing IgG4SD in asbestos-exposed patients.3,11–13 In conclusion, we here describe a clinicopathologically proven case of IgG4SD-related BPF, RF and retroperitoneal fibrosis in an occupationally asbestos-exposed patient, highlighting, as previously suggested, a possible association between these conditions.