Our patient was a 78-year-old man with a diagnosis of diffuse interstitial lung disease (ILD) associated with rheumatoid arthritis treated with methotrexate and prednisone. He was admitted for respiratory failure and new pulmonary infiltrates. The initial diagnostic impression was exacerbation of ILD due to probable respiratory infection, so antibiotic treatment with antipseudomonal coverage began and corticosteroid therapy was increased.
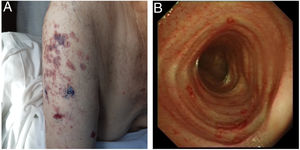
Subsequently, on examination, vesicular, hemorrhagic, bullous, and crusted lesions were observed on the right upper arm and chest, without dermatomal distribution (Fig. 1A), suggestive of disseminated cutaneous herpes zoster, so intravenous acyclovir was initiated. Given the suspicion of varicella zoster virus (VZV) pulmonary involvement, a pharyngeal smear PCR was performed that was positive for VZV, giving a diagnosis of bilateral VZV pneumonia.1 Despite antiviral treatment, fever persisted and acute phase reactant levels increased, so fiberoptic bronchoscopy was performed (Fig. 1B). Pseudomonas aeruginosa was isolated from the bronchial aspirate, so the same antibiotic treatment was maintained. Despite treatment, the patient's progress was poor with radiological progression and respiratory worsening, and he finally died.
Reactivation VZV pneumonia is a rare but fatal complication in patients with ILD.2 Early diagnosis from skin lesions can be vital.