In 1907, Leo Bakeland created Bakelite, the first fully synthetic plastic. During the period surrounding World War II, many new polymers emerged and the plastic industry took off.1 Nowadays, plastic is a versatile and cost-effective material that fulfills many valuable functions in our economy, and daily lives. Unfortunately, the unintended release of plastic into the environment and the mismanagement of plastic waste can be harmful to organisms, the environment, and human health. In 2015, more than 5000 million metric tons of primary plastic waste were produced worldwide, and by 2050, the number is expected to rise up to 25,000 million metric tons.2
Micronanoplastics (MNPs) are small plastic particles formed from larger plastic waste through a process termed weathering. Despite the definition of MNPs has been debated for several years, it can be generalized that microplastics are plastic particles smaller than 5mm across, and nanoplastics are smaller than 1μm in any one dimension.3 Up to now, research has mainly focused on microplastics due to instrumental detection limits and easier manipulation. Nonetheless, during the last years, the harmful effects of microplastics have risen public and scientific awareness; therefore, suitable and optimized detection methods are being developed for nanoplastic research.
The presence of plastics in oceans, seas, freshwater, and soil has been described and studied for decades. However, it was not until 2004 when the term “microplastic” was coined and the presence and effects of MNPs started to be evaluated in other matrices and organisms, respectively.4 MNPs have also been described in the atmosphere, being the main sources a combination of degradation and fragmentation of textiles in indoor air, and tyre and road wear particles in urban outdoor air. MNPs emission to the atmosphere depends on source size and weather processes, which have an impact on their atmospheric transport. In fact, analyses of air mass trajectories showed that MNPs could be transported more than 1000km before being deposited, making urban areas a potential source of microplastics in rural and pristine regions such as the Antarctica.5
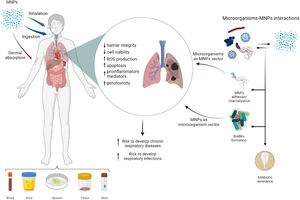
Human and wildlife exposure to MNPs has been already described, however, the impact of this exposure is still not fully elucidated and many gaps need to be filled.3,6 Fortunately, many initiatives and projects are arising on the topic, such as the European Research Cluster to Understand the Health Impacts of Micro- and Nanoplastics (CUSP, https://cusp-research.eu/) in 2020. The main routes of exposure are inhalation, ingestion and, to a lesser extent, dermal contact. Recently, MNPs have been detected in a huge variety of clinical samples, such as blood, urine, feces, milk, placenta, respiratory samples and tissues (Fig. 1).3 Considering that our lungs filter about 12,000L of air a day, we are continuously exposed to different MNPs, and their associated additives, other pollutants, and microorganisms, making the inhalation route of especial concern.7
Numerous microorganisms have the ability to colonize biotic and abiotic surfaces and form biofilms, which can be composed of diverse bacterial, algal, protozoal and fungal species. Thus, plastic debris is an heterogeneous and abundant material suitable for the biofilm-forming microbial communities, which are referred to as “plastispheres”.6 Many studies have reported an enrichment of antibiotic resistant bacteria in plastispheres, and thus horizontal gene transfer might be favored. In addition, resistant microorganisms could be selected upon exposure to MNPs associated with antibiotics.8 Similarly to the effects of cigarette smoke or diesel exhaust particles on some microorganisms, MNPs might have the potential to phenotypically and genotypically redirect microorganisms toward a more virulent profile that could directly impact respiratory infections, their severity, treatment, and prognosis.9–13
Recent studies show that MNPs can interact with microorganisms in a direct manner. It has been seen, that MNPs can attach to bacterial cell surfaces and some can even be internalized. Although these interactions vary between bacterial species and are dependent on the polymer type, size, functional groups and charges, it can be stated that MNPs are strongly associated with microorganisms.14,15 Taking this into consideration, microorganisms could act as vectors of the smallest sized MNPs, which might have a direct effect on infection establishment and progression (Fig. 1).
We are just starting to grasp the huge impact that MNPs have on our health, and more specifically, on our respiratory system. Currently, there are three main mechanisms described by which MNPs affect our respiratory health (Fig. 1). To begin with, our alveolar surface is lined with surfactants that facilitate the gas exchange and aid in the airway clearance. However, when MNPs reach the alveolar air–liquid interface, the surfactant biophysical functions are disrupted and the pulmonary surfactant film collapses. Additionally, some MNPs can deplete tight junction proteins, ultimately causing a disruption of the epithelial cell barrier function. MNPs also cause cytotoxicity in pulmonary epithelial cells, which can be observed by the blebbing morphology and activation of apoptotic pathways.16 What is more, the presence of MNPs in the airways induces epithelial cell inflammation and redox imbalance. Despite many pro-inflammatory cytokines and inflammatory proteins, such as IL-6, IL-8, IL-1β, TGF-β, NF-κβ, are expressed upon MNPs exposure, TNF-α might be one of the most relevant. MNPs seem to deplete antioxidants and increase reactive oxygen species production, which ultimately impacts inflammation processes leading to tissue damage.16–18
Disruption of the lung epithelial barrier and the presence of lung tissue damage, allow many foreign substances and microorganisms to reach the interstitium and bloodstream. Thus, long exposure to MNPs could lead to the development and progression of respiratory diseases such as chronic obstructive respiratory disease, which often presents exacerbations caused by respiratory viruses and bacteria.6,16 In the case of respiratory diseases with unknown cause, such as idiopathic pulmonary fibrosis, exposure to MNPs is proposed as a potential risk factor.
Several studies discuss about the impact of air pollution on the SARS-CoV-2 infection, and the role that MNPs could play on it. SARS-CoV-2 can strongly adhere to MNPs and survive on plastic surfaces for at least 72h. In fact, the virus adsorbed on MNPs has an increased infectivity for target cells in vitro, which ultimately translate into an increased expression of apoptosis and inflammation genes.19 Furthermore, another study demonstrated that MNPs promote influenza A virus (IAV) infection. Several IAV particles can adhere to MNPs, causing an increase of viral particles that get internalized through endocytosis. Additionally, MNPs disrupt the natural antiviral signaling pathway mediated by RIG-I like receptors, worsening the respiratory symptoms and outcome of disease.20
With the growing amount of evidence, it is clear that MNPs have a detrimental effect on our health. This, along with the previous and ongoing research on the impact of MNPs in the environment and animals, clearly brings us to approach the MNPs problematic from a One Health perspective. Despite MNPs are a hot topic at the moment, and a lot of research is being done on its impact on respiratory health, there is still a big gap regarding its impact on respiratory bacterial infections; as research on this topic could shed some light on severe respiratory infections, pathogen persistence, and antibiotic resistance. Additionally, a bigger effort needs to be made for improving detection methods, MNPs characterization, and methodology standardization. Thus, we still have a long way to go before we get enough high-quality data for policy makers to lay down proper regulations on plastic production and plastic waste management.
Funding sourcesFunded projects associated with the content of this editorial: European Union's Horizon 2020 research and innovation Programme under Agreement No. 965196 (PLASTICHEAL); Instituto de Salud Carlos III (PI22/01834) incorporated into the National Plan for R+D+I, co-funded by the ISCIII-Subdirectorate-General for Evaluation and the European Regional Development Fund (ERDF), and by the CERCA Program of the Government of Catalonia.
Conflict of InterestsThe authors state that they have no conflict of interests.