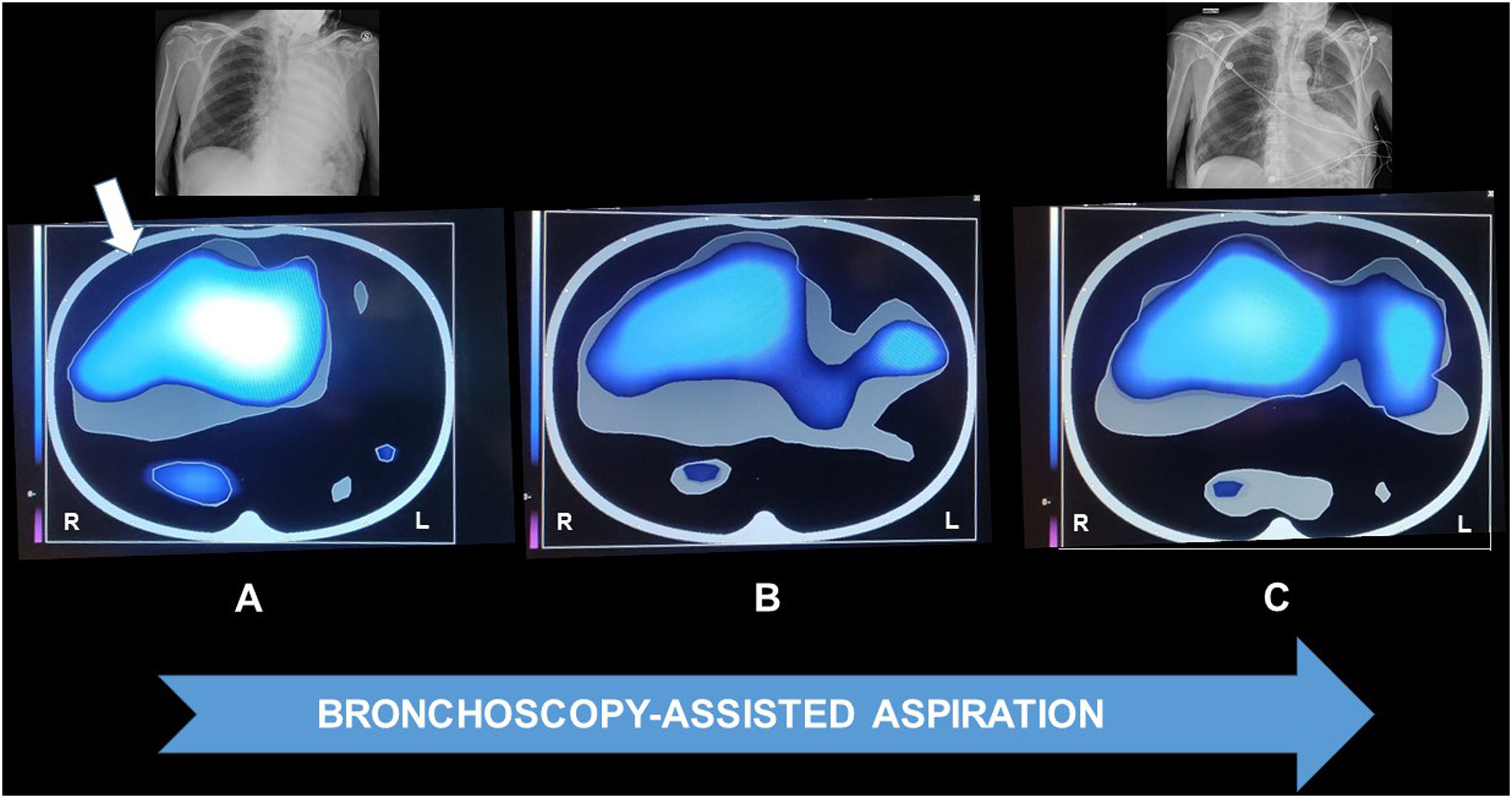
A 79-year-old male with Parkinson's disease was admitted to the hospital for acute clinical deterioration caused by severe left lung aspiration pneumonia. In view of worsening hypoxemia and evidence from the CXR of the left “white” lung (Fig. 1), the patient was ordered a bronchoscopy-assisted tracheobronchial aspiration (BAA). Images were continuously provided by electrical impedance tomography (EIT) during the BAA permitting the physician to assess changes in the distribution of ventilation. The EIT showed a partial re-expansion of the left lung during the procedure, which was confirmed by a bedside CXR (Fig. 1).
Images obtained by electrical impedance tomography before bronchoscopy-assisted tracheobronchial aspiration was initiated (A), during the procedure (B), and immediately after its conclusion (C). At the start of the procedure, a clear unilateral distribution of ventilation is present (white arrow). The blue–white gradient indicates regional distribution of tidal ventilation. In the upper part chest X-rays carried out before and immediately after the procedure are shown (L=left; R=right).
Chest X-rays (CXR) and/or computed tomography (CT) scans are commonly used to assess lung ventilation in this type of patient, but both generate static images that are unable to detect changes occurring during procedures and treatments. Although lung ultrasound can visualize dynamic changes during breathing cycles, it can only produce images of the area under the probe.1
EIT, a non-invasive monitoring tool, can instead provide continuous transverse images of the lungs, allowing a breath-to-breath bedside evaluation of lung ventilation which can facilitate early recognition of serious events such as atelectasis, pneumothorax and pleural effusions.2
Our data demonstrate that EIT can detect lung re-expansion and help physicians to perform a reliable BAA in cases of unilateral severe pneumonia.
Conflict of interestNone.