We performed a systematic literature review and meta-analysis to assess the efficacy and safety of single-inhaler triple therapy (SITT) compared to monotherapy, dual therapy, and open TT (OTT), at 52 weeks, in five predefined subgroups of moderate/severe COPD patients (see supplementary material).
We included nine articles from five randomized controlled trials of good quality.1–9 The studies analyzed mortality,3,4 rate of moderate and severe exacerbations,2,5–10 changes in the FEV1,1,6,8,9 dyspnea (using the Transition Dyspnea Index [TDI]),6 and quality of life (using the St. George's Respiratory Questionnaire [SGRQ]).1,6,9
Previous Exacerbation HistoryIn the FULFIL trial, SITT was associated with a lower rate of moderate-to-severe exacerbations than LABA/ICS in patients with ≥1 severe exacerbation (p<0.05), but there were no differences in patients with ≥2 moderate exacerbations. Besides, SITT significantly improved trough FEV1 compared to LABA/ICS in patients with ≥2 moderate exacerbations (difference: 199ml) or ≥1 severe exacerbation (difference: 166ml), but also in those with FEV1 ≥50–<80% and ≥2 moderate exacerbations or ≥1 severe exacerbation (difference: 179ml).1 However, improvements in SGRQ with SITT compared to LAMA/ICS were only statistically significant (p=0.026) in patients with ≥2 moderate exacerbations.1
The IMPACT trial found that SITT in patients with ≥2 moderate/severe exacerbations resulted in a reduction in the annual rate of exacerbations compared to LABA/ICS (difference: 11%, p<0.01) and LAMA/LABA (difference: 28%, p<0.001).2 But in the TRIBUTE study, there was no difference in the exacerbation rate between SITT and LAMA/LABA in patients with >1 exacerbation.5
The ETHOS trial compared SITT at two ICS dose levels with LABA/ICS and LAMA/LABA.7 Except for SITT at the low ICS dose level, the rate of moderate or severe exacerbations was significantly lower with SITT than with LABA/ICS and LAMA/LABA in patients with ≥2 exacerbations.7 Another analysis reported a significantly lower risk of death with SITT compared to LAMA/LABA in patients with ≥2 moderate or severe exacerbations: HR=0.36 (95% CI 0.19–0.70) and HR=0.55 (95% CI 0.32–0.97) for SITT at high (320μg) and low (160μg) ICS dose levels.4 No differences were observed compared to LABA/ICS in patients with ≥1 severe exacerbation.4
The TRINITY study, which included patients with severe and very severe COPD,8 reported that SITT compared with LAMA and OTT significantly decreased the rate of moderate or severe exacerbations in patients with >1 exacerbation (RR=0.72, and RR=0.71).8
Lung Function and COPD SeverityThe FULFIL study showed that SITT significantly improved FEV1 at 52 weeks compared to LABA/ICS in patients with FEV1 ≤50% and ≥1 moderate or severe exacerbation (difference: 140ml). The difference was larger (224ml) in patients without a history of exacerbations.1 No statistical differences in the SGRQ were observed between groups.
A sub analysis of the ETHOS trial revealed that mortality was significantly lower in patients with FEV1 <50% on SITT at the high ICS dose level (320μg) compared to LAMA/LABA. However, no differences were observed between SITT at both dose levels and LABA/ICS and between SITT at the 160μg dose level and LAMA/LABA.4
In the TRINITY study,8 SITT significantly reduced the rate of moderate or severe exacerbations (HR=0.77, p<0.050) compared to LAMA, yet not in patients with very severe COPD. Similar findings were reported for changes in FEV1. However, there were no differences between SITT and OTT regarding the rate of exacerbations and changes in FEV1 in patients with severe or very severe COPD.
Blood Eosinophil ConcentrationThe IMPACT trial showed that in patients with eosinophil levels ≥150cells/μL, the rate of moderate–severe exacerbations was significantly lower with SITT compared to LABA/ICS and LAMA/LABA, amounting to 0.95%, 1.08%, and 1.39%, respectively.2 Yet, SITT was only statistically superior to LABA/ICS and not to LAMA/LABA in patients with <150cells/μL.2
In the ETHOS trial,7 the rate of moderate or severe exacerbations was significantly lower with SITT (high and low ICS dose levels) than with LABA/ICS and LAMA/LABA in patients with eosinophil counts ≥150cells/μL. In patients with <150cells/μL, both SITT dose levels were significantly superior to LABA/ICS, but no differences were observed with LAMA/LABA.
The IMPACT trial explored the rate of exacerbations and the changes in SGRQ, FEV1, and TDI on SITT compared to LAMA/LABA according to different eosinophil level cut-offs (90, ≥90–<140, ≥140–<200, ≥200–<310, and ≥310cells/μL). In general, the magnitude of the benefit on SITT increased proportionally to blood eosinophil count, though the relationship with FEV1 was less marked.6
In the TRIBUTE study,5 the annual rate of moderate/severe exacerbations was significantly lower on SITT than on LAMA/LABA in patients with eosinophil levels ≥2%, while there were no differences between treatments for levels <2%.5
In the TRINITY trial,8 in which patients with eosinophil levels ≥2% had a lower risk of moderate or severe exacerbations with SITT than with LAMA (RR=0.70, p<0.050), there were no differences in patients with eosinophil levels <2%. On the other hand, changes in FEV1 were significantly greater with SITT than with LAMA in both eosinophil level subgroups (0.07L, and 0.04L, respectively). However, when comparing SITT with OTT, there were no differences in the rate of exacerbations and FEV1 changes in any eosinophil level subgroups.8
Smoking StatusIn the IMPACT trial, the reduction in the annual exacerbation rates was significantly more pronounced with SITT than with LABA/ICS and LAMA/LABA, regardless of smoking status.2 In current smokers, the reduction rates compared to dual therapies were 15% (p<0.01) and 14% (p<0.05), respectively. In former smokers 15% (p<0.001) and 30% (p<0.001).2 Smoking status had also an impact on several variables, including moderate or severe exacerbations, TDI, and FEV1, depending on blood eosinophil count.6
In the TRIBUTE trial, the reduction in the rate of moderate or severe exacerbations was significantly greater with SITT than with LAMA/LABA in current smokers (RR=0.77), without differences in former smokers.5
In the TRINITY study, the risk of moderate or severe exacerbations was lower with SITT than with LAMA in current smokers (RR=0.76, p<0.050), with no differences in former smokers.8 On the other hand, changes in FEV1 were significantly more marked with SITT than with LAMA in current smokers (difference 0.06L, p<0.050) and in former smokers (difference 0.06L, p<0.050).
There were no differences between SITT and OTT in the rate of exacerbations and FEV1 changes in current and former smokers.8
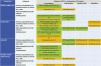
Previous Medications (Table 1)Summary of the Main Results of the Meta-analysis at 52 Weeks. Green Color Represents Comparisons With Higher Level of Evidence in Favor of Single-inhaler Triple Therapy (Meta-analysis or Clear Effect From Randomized Clinical Trials). Yellow Color Depicts Contradictory Results or an Absence of Difference Between Treatment Groups Across Several Comparisons. Light Blue Color Indicates Lacking Data. For Each Result the Study References are Provided.
Abbreviations: SITT: single-inhaler triple therapy; FEV1: forced expiratory volume in 1 second; μL: microliter; LAMA: long-acting muscarinic antagonists; LABA: long-acting β2-agonists; ICS: inhaled corticosteroids; HR: hazard ratio; CI: confidence interval.
1. Vestbo J, Papi A, Corradi M, Blazhko V, Montagna I, Francisco C, et al. Single inhaler extrafine triple therapy versus long-acting muscarinic antagonist therapy for chronic obstructive pulmonary disease (TRINITY): a double-blind, parallel group, randomized controlled trial. Lancet. 2017;389(10082):1919–29.
2. Martinez FJ, Rabe KF, Ferguson GT, Wedzicha JA, Singh D, Wang C, et al. Reduced all-cause mortality in the ETHOS trial of budesonide/glycopyrrolate/formoterol for COPD: a randomized, double-blind, multi-center parallel-group study. Am J Respir Crit Care Med. 2020.
3. Papi A, Vestbo J, Fabbri L, Corradi M, Prunier H, Cohuet G, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomized controlled trial. Lancet. 2018;391(10125):1076–84.
4. Lipson DA, Barnhart F, Brealey N, Brooks J, Criner GJ, Day NC, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378(18):1671–80.
5. Rabe KF, Martinez FJ, Ferguson GT, Wang C, Singh D, Wedzicha JA, et al. Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. N Engl J Med. 2020;383(1):35–48.
6. Pascoe S, Barnes N, Brusselle G, Compton C, Criner GJ, Dransfield MT, et al. Blood eosinophils and treatment response with triple and dual combination therapy in chronic obstructive pulmonary disease: analysis of the IMPACT trial. Lancet Respir Med. 2019;7(9):745–56.
7. Axson EL, Lewis A, Potts J, Pang M, Dickinson S, Vioix H, et al. Inhaled therapies for chronic obstructive pulmonary disease: a systematic review and meta-analysis. BMJ Open. 2020;10(9):e036455.
8. Halpin DMG, Birk R, Brealey N, Criner GJ, Dransfield MT, Hilton E, et al. Single-inhaler triple therapy in symptomatic COPD patients: FULFIL subgroup analyses. ERJ Open Res. 2018;4(2).
In the FULFIL trial, SITT was statistically superior to LABA/ICS in reducing exacerbations in patients previously on LABA/ICS and OTT.1 Improvements in FEV1 were greater with SITT irrespective of previous medications, but there were no differences when changes in quality of life were analyzed.1
Post hoc data from the IMPACT study showed that in patients on ICS at screening, mortality was significantly lower with SITT compared to LAMA/LABA (HR=0.63, 95% CI 0.44–0.89), but no differences were found compared to ICS/LABA.3 Besides, the risk of death with SITT compared to LAMA/LABA in patients on OTT at screening was HR=0.40 (95% CI 0.19–0.84).3 The reduction in moderate or severe exacerbations was also greater in the SITT group than in the LAMA/LABA group in patients on ICS, LABA/ICS, or OTT at screening, yet with no statistically significant differences in patients with previous LAMA or LAMA/LABA.9
In the ETHOS trial, there were no differences in mortality between SITT and LABA/ICS in patients with prior ICS or OTT.4 However, this risk was significantly lower on SITT at the high ICS dose level (budesonide 320μg) than on LAMA/LABA in patients with previous ICS or OTT.4
We did not identify any safety data specifically in the subgroups analyzed.
In the meta-analysis (Table 2) we found that in patients with ≥2 moderate and/or ≥1 severe exacerbations, SITT resulted in greater reductions in the annual rate of exacerbations compared to LAMA/LABA (HR=0.73, 95% CI 0.67–0.79), without relevant heterogeneity.4,5 Similar results were observed in patients with high eosinophil levels (HR=0.70, 95% CI 0.65–0.76), yet with a high and significant heterogeneity (I2=74.3%, p=0.020). There was also a relevant heterogeneity (I2=83.2%, p=0.003) in the rate of exacerbations in patients with high eosinophil levels when comparing SITT and LABA/ICS (HR=0.82, 95% CI 0.76–0.87).
Main Results of Single-inhaler Triple Therapy at 52 Weeks According to COPD Medication at Screening. Green Color Represents Comparisons With Statistically Significant Evidence in Favor of Single-inhaler Triple Therapy. Yellow Color Depicts Contradictory Results or an Absence of Difference Between Treatment Groups. Light Blue Color Indicates Lacking Data.
Abbreviations: COPD: chronic obstructive pulmonary disease; LAMA: long-acting muscarinic antagonists; LABA: long-acting β2-agonists; ICS: inhaled corticosteroids; SITT: single-inhaler triple therapy; BF: budesonide/formoterol; FEV1: forced expiratory volume in 1 second; ml: milliliter; SGRQ: St. George's Respiratory Questionnaire; Dif.: difference; HR: hazard ratio; CI: confidence interval.
1. Halpin DMG, Birk R, Brealey N, Criner GJ, Dransfield MT, Hilton E, et al. Single-inhaler triple therapy in symptomatic COPD patients: FULFIL subgroup analyses. ERJ Open Res. 2018;4(2).
2. Han MK, Criner GJ, Dransfield MT, Halpin DMG, Jones CE, Kilbride S, et al. The effect of inhaled corticosteroid withdrawal and baseline inhaled treatment on exacerbations in the IMPACT study. A randomized, double-blind, multicenter clinical trial. Am J Respir Crit Care Med. 2020;202(9):1237–43.
3. Rabe KF, Martinez FJ, Ferguson GT, Wang C, Singh D, Wedzicha JA, et al. Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. N Engl J Med. 2020;383(1):35–48.
4. Lipson DA, Crim C, Criner GJ, Day NC, Dransfield MT, Halpin DMG, et al. Reduction in all-cause mortality with fluticasone furoate/umeclidinium/vilanterol in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2020;201(12):1508–16.
5. Martinez FJ, Rabe KF, Ferguson GT, Wedzicha JA, Singh D, Wang C, et al. Reduced all-cause mortality in the ETHOS trial of budesonide/glycopyrrolate/formoterol for COPD: a randomized, double-blind, multi-center parallel-group study. Am J Respir Crit Care Med. 2020.
In conclusion, SITT results in more pronounced clinical benefits on exacerbations and lung function compared to other inhaled COPD medications in patients with moderate-to-severe COPD, especially in those at high risk of exacerbations and with high blood eosinophil concentrations. Further evidence (in the long-term, daily practice, etc.) is needed to fully capture the characteristics of patient subgroups that may benefit most from SITT and to identify those with a substantial extra safety risk.
Ethical ApprovalThis study was performed in line with the principles of the Declaration of Helsinki.
Authors’ ContributionsThe study was conceived by all authors, all were involved in the study planning and design. JAR was involved in study delivery, prepared the data and carried out statistical analysis. All authors provided expert opinion on development of the analysis and interpreting the data. JAR and BC developed and wrote the manuscript, with critical revisions and review of the final manuscript from all other authors.
FundingThe study was funded by an unrestricted educational grant from Chiesi.
Conflict of InterestThe authors declare no conflicts of interest.