Journal Information
Vol. 61. Issue 4.
Pages 189-190 (April 2025)
Share
Download PDF
More article options
Vol. 61. Issue 4.
Pages 189-190 (April 2025)
Editorial
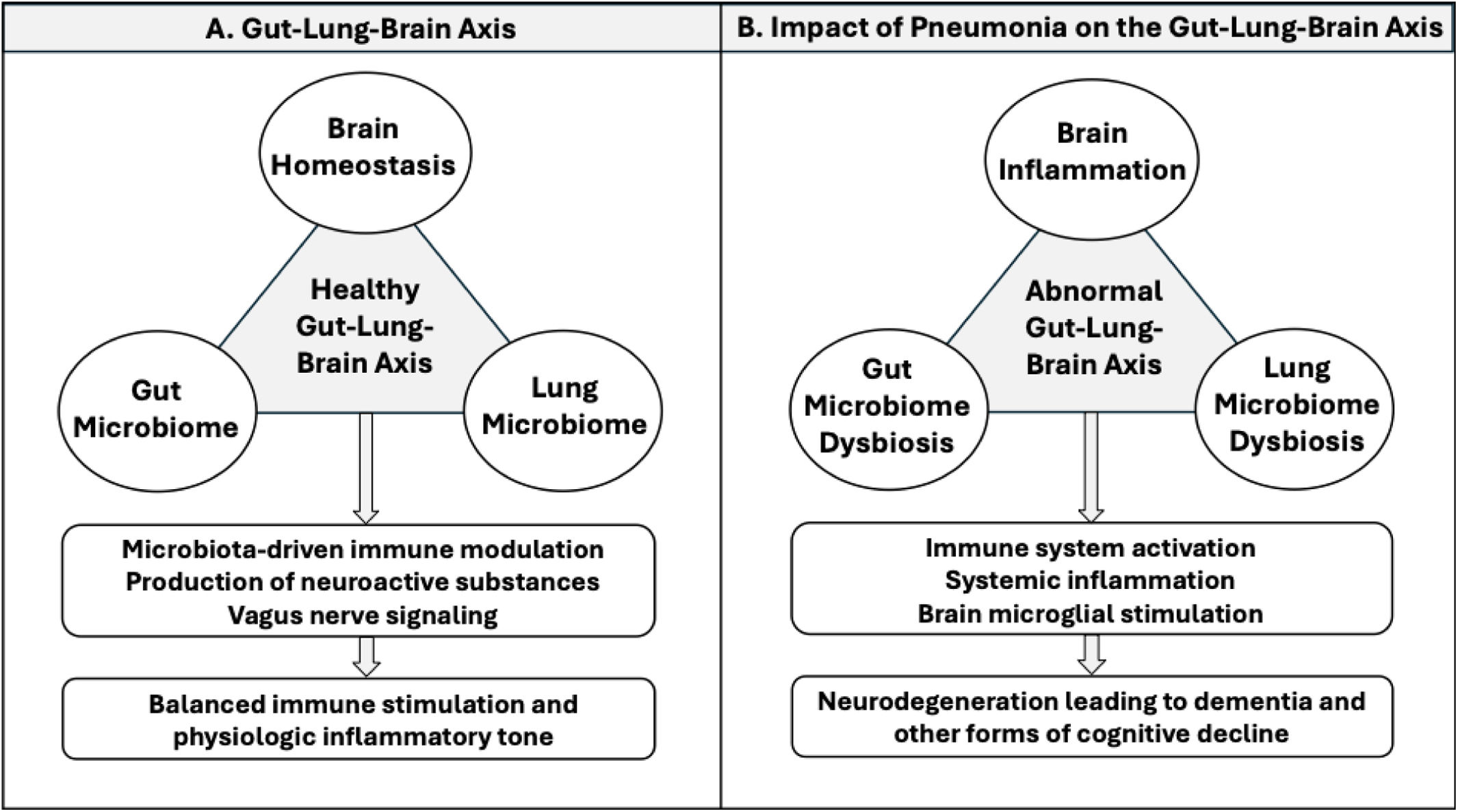
Cognitive Decline in Pneumonia: A Neglected Consequence
Visits
1431
This item has received
Article information
These are the options to access the full texts of the publication Archivos de Bronconeumología