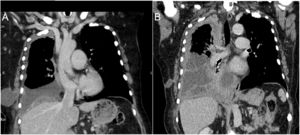
A 73-year-old lady diagnosed with right-sided malignant pleural effusion (MPE) secondary to breast cancer underwent video-assisted thoracoscopic surgery (VATS) for pleurodesis. Unfortunately, pleurodesis was unsuccessful and the patient experienced recurrence of the symptomatic effusion. A computed tomography (CT) scan done four weeks after the surgery revealed the development of a subcutaneous pocket of fluid (Fig. 1A), presumably at the site of one of the surgery ports. The effusion was not amenable to aspiration due to heavy septations. CT scan done 8 weeks later showed the diminution of the size of the chest wall pocket with increase in the size of the effusion (Fig. 1B) with ongoing breathlessness. Ultrasound examination revealed a new anterior free pleural collection. An indwelling pleural catheter (IPC) was inserted with considerable symptomatic improvement.
(A) A coronal CT image shows right sided-pleural effusion and ipsilateral fluid-containing cyst in the chest wall. (B) CT image shows partial resolution of the chest wall collection with increase in pleural thickening (particularly in the apex) as well as the pleural effusion. Note dense septations inside the fluid.
The development of a chest wall seroma as a complication of thoracic surgery is very uncommon and is reported in less than 1% of thoracotomies, but it is not a recognized complication of VATS.1 However, this complication was reported following simpler procedures breeching the pleural space such as thoracentesis2 and IPC insertion.3