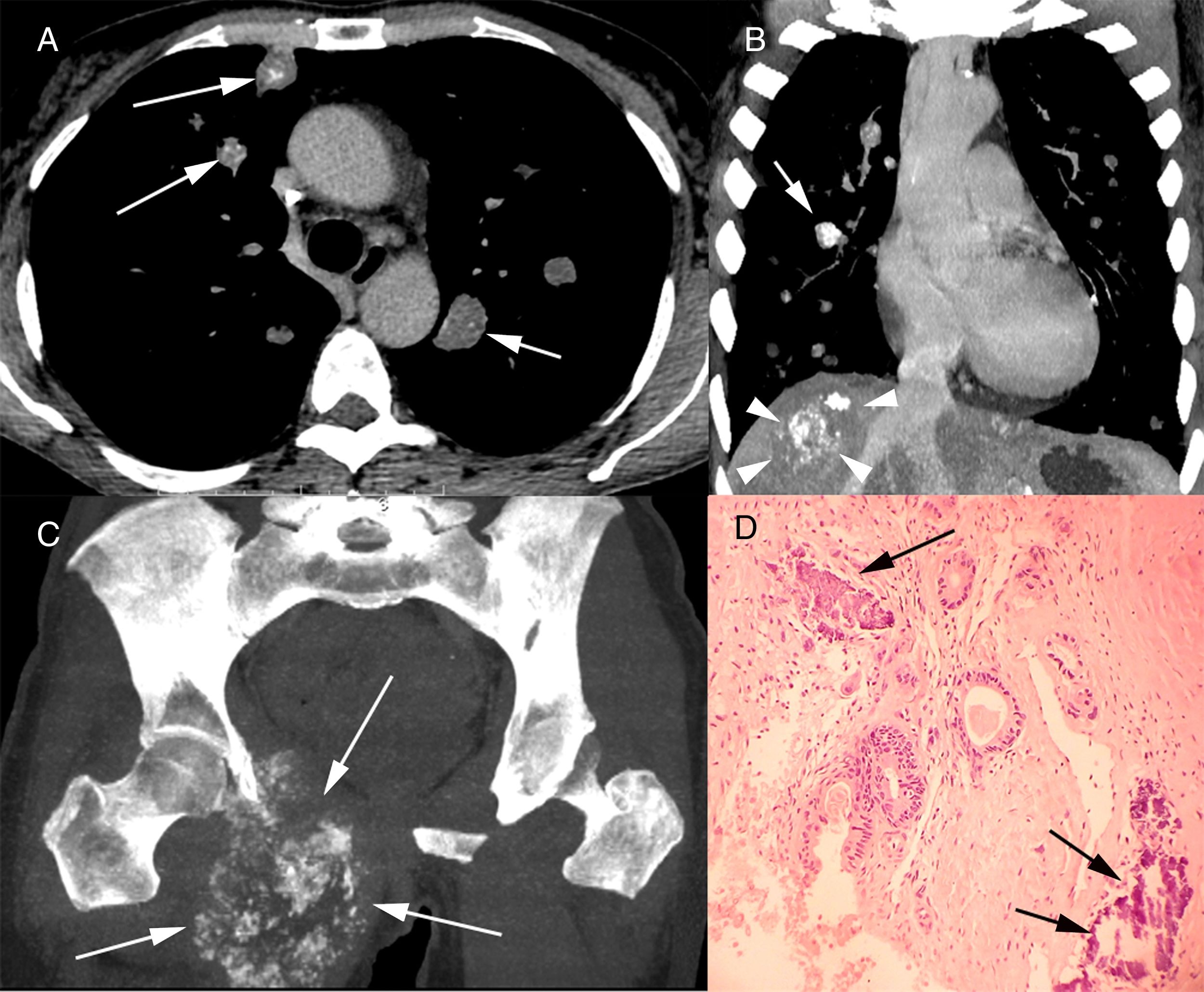
A 50-year-old female patient underwent thoracic and abdominal computed tomography examinations for oncological follow-up. The images showed multiple lung nodules, some of which were calcified (Fig. 1A and B), a calcified hepatic mass, and an expansile osteolytic lesion with internal foci of calcification on the ischiopubic ramus of the right hip (Fig. 1C). The patient had undergone colonoscopy 3 years previously due to rectal bleeding, which showed an exophytic and stenosing rectal lesion. The biopsy findings were compatible with well-differentiated tubular adenocarcinoma. Surgical resection confirmed the anatomopathological diagnosis and identified vascular and perineural invasion with metastasis to the peritumoral lymph nodes. The patient started chemotherapy at that time. Our main question was whether the new lesions were metastases of the rectal tumor or corresponded to a new tumor (e.g., bone sarcoma with pulmonary and hepatic metastases), which would imply the need to change the treatment strategy. Biopsies of the bone lesion and a pulmonary nodule were performed, and showed metastatic adenocarcinoma with a tubuloacinar pattern (Fig. 1D).
Chest computed tomography with axial (A) and coronal (B) reconstruction showing multiple pulmonary nodules, some with calcification (arrows). Note also in B a calcified mass in the right lobe of the liver (arrowheads). In C, computed tomography of the pelvis with coronal acquisition MIP reconstruction, showing an osteolytic lesion with internal foci of calcification (arrows) and invasion of surrounding soft tissue. In D, histological section of the pulmonary nodule demonstrating atypical neoplastic glands infiltrating the connective tissue amid desmoplastic stroma. Note also the amorphous basophilic material, compatible with extracellular deposition of calcium adjacent to the neoplastic process (arrows; hematoxylin and eosin stain, ×100).
Calcification of a pulmonary nodule is usually suggestive of its benign nature – such nodules are most commonly granulomas and less commonly hamartomas – but calcification and ossification can also occur in malignant lesions. Multiple pulmonary nodules have numerous etiologies, but the diagnostic possibilities are considerably reduced when these lesions show calcification. The main diagnostic considerations are calcified pulmonary metastases, amyloidosis, hyalinizing granulomas, epithelioid hemangioendothelioma, necrobiotic nodules, and multiple chondromas. Amyloidosis, in its nodular form, is usually asymptomatic. The definitive diagnosis is made by histopathology, on the basis of the finding of deposition of amyloid, which stains with Congo red and shows apple-green birefringence under polarized light. Hyalinizing granulomas are rare fibrotic pulmonary lesions, usually associated with autoimmune phenomena related mainly to exposure to mycobacterial or fungal antigens. Epithelioid hemangioendothelioma is a rare multifocal pulmonary neoplasm of endothelial origin. It is considered to be a sarcoma of low aggressiveness. Necrobiotic nodules can develop in patients with pneumoconiosis associated with rheumatoid arthritis. Calcification in pulmonary chondromas is a common radiological finding. The association of these chondromas with gastrointestinal stromal tumors and extra-adrenal paragangliomas is known as the Carney triad.1–3
The calcification of pulmonary metastases is very uncommon. The tumors that most commonly give rise to calcified metastases are sarcomas (osteosarcoma, chondrosarcoma, synovial sarcoma, and giant cell tumor of the bone), carcinomas (particularly mucinous and papillary adenocarcinomas), and treated metastatic choriocarcinoma. Several mechanisms are responsible for the calcification of metastases: bone formation in tumor osteoid in osteosarcoma; calcification and ossification of tumor cartilage in chondrosarcoma; dystrophic calcification in papillary carcinoma of the thyroid, giant cell tumor of the bone, synovial sarcoma, and treated metastatic tumors; and mucoid calcification in mucinous adenocarcinoma of the gastrointestinal tract and breast. Calcification can develop in metastases of several other tumors after chemotherapy or radiotherapy, generally secondary to degeneration, hemorrhage, and necrosis.1,4,5 Although tubular-type adenocarcinoma is not listed among the major causes of calcified metastases, the patient described here had undergone previous chemotherapy, which may have been the mechanism for calcification formation.