Secondary spontaneous pneumothorax always develops secondary to underlying lung disease. Although its occurrence due to cancer is rare, it is mainly related to sarcomas. Bilateral pneumothorax is less common. Pazopanib, used in the treatment of sarcoma patients, is also a cause of pneumothorax. Pazopanib, a tyrosine kinase inhibitor, is frequently used for renal cell carcinoma, pancreatic neuroendocrine tumors, and especially soft tissue sarcomas. Pneumothorax cases due to pazopanib have been reported in the literature.1,2
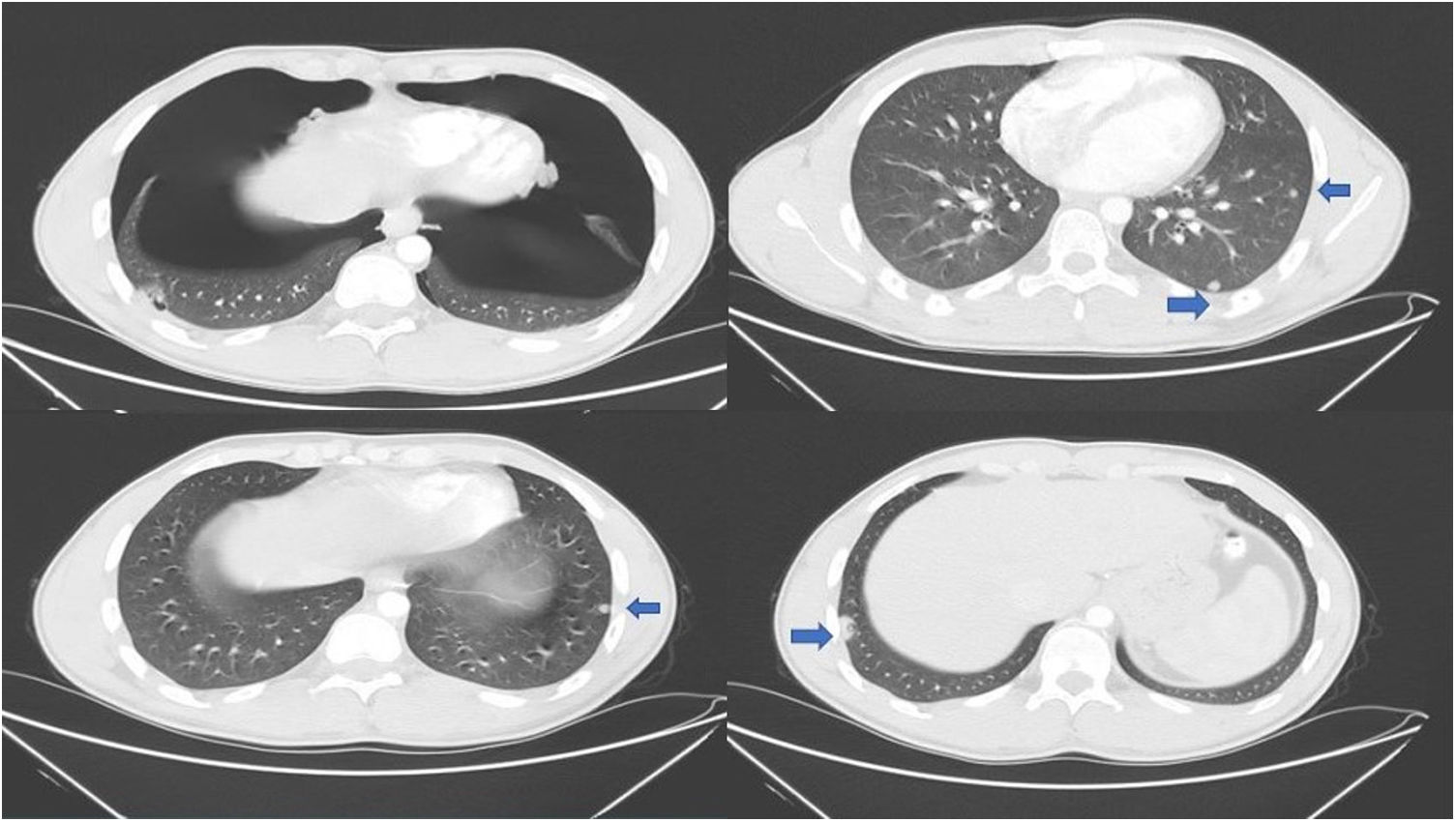
An 18-year-old male patient was admitted to the hospital with a palpable approximately 10cm mass lesion on the lateral side of the gastrocnemius muscle of the left lower extremity. The mass of the patient who did not detect distant metastases as a result of positron emission tomography (PET/CT) was surgically excised. As a result of the pathological evaluation of the material removed after the operation, it was reported that the mass was synovial sarcoma. Six courses of IMA (ifosfamide, mesna, adriamycin) treatment was planned. Six months after the completion of adjuvant therapy, multiple lung nodules were detected on thoracic computed tomography (CT). New systemic treatment was planned for the patient for recurrent synovial sarcoma. Primary granulocyte colony-stimulating factor (G-CSF) prophylaxis with gemcitabine and docetaxel treatment was planned as second-line chemotherapy. Despite the primary prophylaxis, the patient could not tolerate chemotherapy due to deepening bi-cytopenia, and the patient's systemic treatment was discontinued due to toxicity. Pazopanib was started as a third-line treatment. The radiologic evaluation was performed after 3 months of treatment in the patient, who did not detect any toxicity with pazopanib treatment and did not have any complaints. Bilateral significant pneumothorax was detected in the CT performed to evaluate the response. Diffuse bilateral pneumothorax is shown in Fig. 1. Despite bilateral significant pneumothorax, the patient did not have any clinical deterioration. The patient was treated with tube thoracostomy and he was discharged after five days of hospitalization. Pazopanib was restarted at 400mg/day for two weeks after discharge. Systemic treatment of the patient who developed pneumothorax again after one week of pazopanib use was completely discontinued.
Soft tissue sarcomas metastasize quite frequently. The lung is an important site of metastasis. Unfortunately, treatment options are limited in metastatic soft tissue sarcomas. Pazopanib is an effective treatment option for these patients. In a pre-approved clinical study of pazopanib for metastatic soft tissue sarcoma, the incidence of pneumothorax during pazopanib treatment was reported to be approximately 2%.3 However, higher pneumothorax rates (∼10%) have also been reported in more recent studies.4 The mechanism of secondary pneumothorax arising from lung metastases is not clear. However, various theories such as tumor necrosis, check valve and tumor embolism have been reported.4 In addition, it is well known that angiogenesis inhibitors cause tumor necrosis and cavitation in lung lesions.5 Pazopanib can also cause pneumothorax by using this mechanism of action. Especially in sarcoma patients with diffuse lung metastases, routine lung examination and chest X-ray should be planned even if there are no symptoms while using pazopanib treatment.
FundingNo funders pertaining to this article.