Mycobacterium avium management still remains a challenge today, given the ease with which antimicrobial resistance and adverse effects of combination therapy occur.1 Bedaquiline and delamanid have been shown to be very effective in the treatment of drug-resistant tuberculosis.2 Both drugs have very good in vitro activity against most nontuberculous mycobacteria (NTM).3 Moreover, several articles have already shown bedaquiline to be effective in their presentation.4,5 However, no experience with delamanid in the treatment of NTM has been published.
We present the case of a 46-year-old male diagnosed with stage C3 HIV infection in June 2020. He started antiretroviral treatment (ART) and six months later was admitted to our hospital due to abdominal pain. (CD4: 54cells/mm3, HIV viral load: undetectable). Computed tomography showed an abdominal mass formed by multiple mesenteric and retroperitoneal lymphadenopathies. Biopsy of the adenopathies showed growth of M. avium, and no mutations associated with resistance to clarithromycin, amikacin or rifampicin were detected. Treatment was started with rifampicin, azithromycin, and ethambutol.
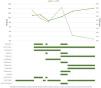
In April 2021 he was admitted again because of abdominal pain. Gastroscopy was performed and showed duodenal mucosa with biopsy reported as granulomatous inflammation, possibly due to MNT. Considering the possibility of treatment failure, it was decided to boost the treatment by adding amikacin (three weeks) and levofloxacin. In view of his good clinical evolution, he was discharged from hospital in July 2021 on azithromycin, levofloxacin, and ethambutol, withdrawing rifampicin due to interactions with the ART (Fig. 1).
He was readmitted for abdominal pain and weight loss in October 2021 and required treatment with morphine for pain control; blood tests showed C-reactive protein 7.4mg/dL and hemoglobin 9.5g/dL. Abdominal computed tomography showed an increase in the mesenteric lymph node mass with partial necrosis. Blood cultures drawn in May, July, and October 2021 showed M. avium growth. The patient claimed to have taken all the medication, so it was accepted that he presented a therapeutic failure to the schemes used, and a resistance study was performed and reported: clarithromycin MIC=4g/ml (sensitive), moxifloxacin MIC 8g/ml (resistant), and linezolid=32g/ml (resistant). Mutations associated with resistance to clarithromycin, amikacin, and rifampicin were still not detected. Compassionate use of bedaquiline and delamanid was requested, as well as an extended sensitivity study to these drugs in order to build a new rescue therapeutic regimen. While waiting for pharmacy approval, he started treatment with seven drugs: azithromycin, amikacin, meropenem, linezolid, rifampicin, moxifloxacin and cycloserine. After confirming susceptibility to delamanid (MIC=0.5mg/dL) and bedaquiline (MIC=0.06mg/dL), a new therapeutic treatment was prescribed in January 2022 with azithromycin, cycloserine, bedaquiline (400mg/day for two weeks followed by 200mg three times a week), delamanid (100mg every 12h), and meropenem. After one month of treatment the patient presented a decrease in pain, reduction of inflammatory parameters, disappearance of anemia, negativization of blood cultures, and improvement in nutritional status. He was discharged at the end of February 2022 with azithromycin, cycloserine, bedaquiline, and delamanid; the treatment that he maintains at present (Fig. 1). He has required weekly ECG monitoring without presenting QT interval lengthening.
In our patient, bedaquiline and delamanid were administered on a compassionate use basis due to the ineffectiveness of other drugs commonly used in the treatment of M. avium. Both drugs allowed a scheme to be established that has proved to be highly effective, with no evidence of resistance or cardiological toxicity to date. Our experience supports the use of bedaquiline and delamanid in salvage treatments in patients with disseminated M. avium for whom there is no other therapeutic alternative.
FundingThere is no funding related to this article.
Conflict of interestsThe authors state that they have no conflict of interests.