A 60-year-old man underwent circumferential radiofrequency catheter ablation of the pulmonary veins to treat atrial fibrillation. The patient evolved without symptoms for the next 2 weeks. Eighteen days after the procedure, he sought emergency care due to chest discomfort and fever. He evolved with a significant decrease in consciousness level (Glasgow Coma Scale score of 3).
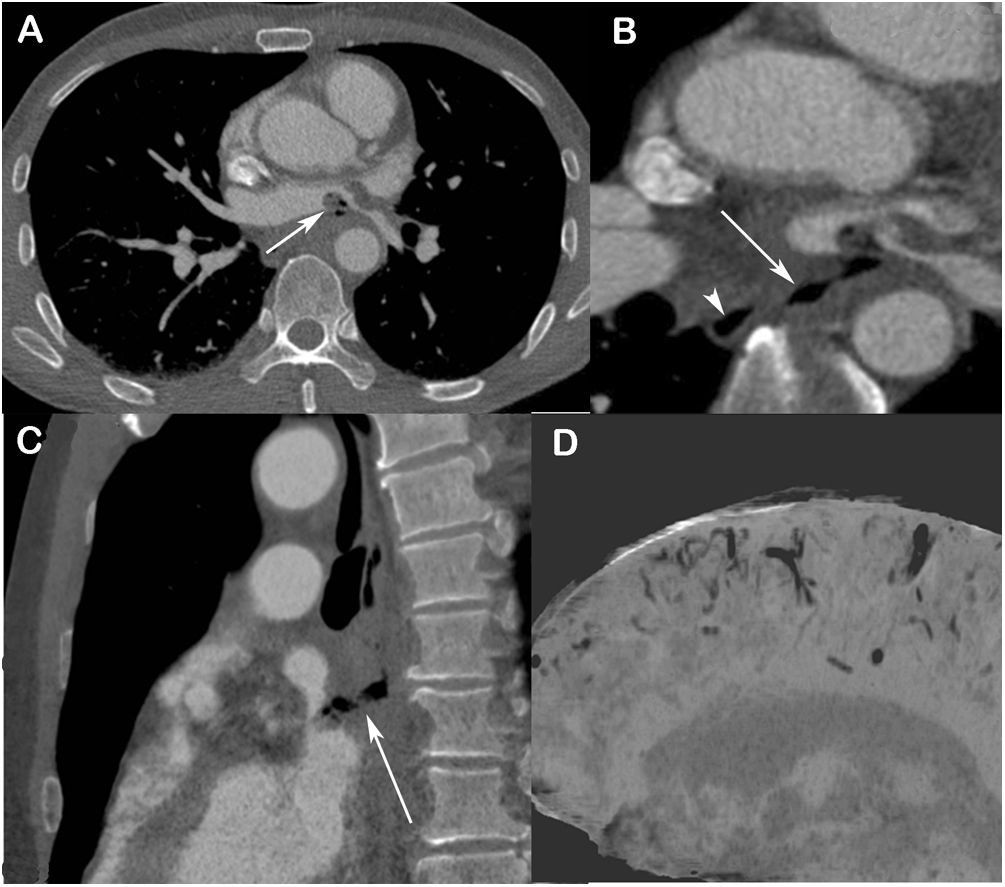
Chest computed tomography (CT) demonstrated a fistulous tract comprising an air passage communicating the middle esophageal wall with the left inferior pulmonary vein ostium. The diagnosis of atrioesophageal fistula (AEF) was made. A rounded feature suggestive of thrombus projecting into the left atrium was also observed (Fig. 1A–C). Brain CT revealed gas content in the leptomeningeal spaces, filling the grooves between the cortical gyri, comprising gas embolism (Fig. 1D).
(A and B) Contrast-enhanced axial chest computed tomography images obtained with the mediastinal window setting, showing (A) a filling defect inside the left atrium (arrow) compatible with a thrombus and associated with gaseous foci, and (B) an air trajectory compatible with a fistula (arrow) communicating with the esophagus, located to the right of the spine (arrowhead) and the ostium of the left inferior pulmonary vein. In C, oblique reconstruction highlights the anteroposterior fistulous tract (arrow) between the esophagus and left atrium. In D, sagittal minimum-intensity projection reconstruction of an image of the brain reveals signs of leptomeningeal gas embolism.
The patient underwent surgical intervention, with raphy of the atrium. A conservative approach was adopted in relation to the esophagus. He developed severe septic shock and died about 4 days after diagnosis.
Catheter ablation has been established as an important treatment for symptomatic atrial fibrillation, leading to significant improvement in patients’ quality of life. AEF is a rare but serious complication of atrial fibrillation catheter ablation, with high mortality rates.1,2 Massive air embolism, especially when multifocal, should raise the suspicion of AEF at initial medical contact.1
Conflicts of interestThe authors declare that they have no conflicts of interest to express.