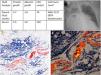
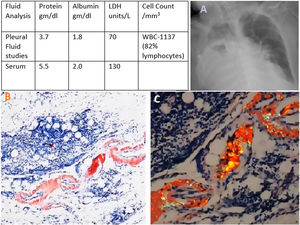
Amyloidosis is extracellular tissue deposition of fibrils composed of variety of proteins. Different types include AA, AL and ATTR. An 82-year-old lady with history of AL type primary amyloidosis and chronic systolic heart failure presented to the hospital following a mechanical fall. Initial imaging studies showed multiple pelvic fractures and a moderate to large right sided pleural effusion. She underwent closed reduction and percutaneous fixation of her pelvic fractures. Post-procedure course was complicated by persistent hypoxia following which right sided thoracentesis was performed and 1000cc of serosanguinous pleural fluid removed. Fluid analysis revealed a non-diagnostic exudative effusion (Fig. 1 table A). Patient underwent medical thoracoscopy with pleural biopsies and chest tube placement. Biopsy was consistent with amyloidosis (Fig. 1 B, C). Pulmonary amyloidosis develops in 1–2% of patients with systemic amyloidosis and can present with tracheobronchial infiltration, persistent pleural effusions (pleural amyloid deposits), parenchymal nodules (amyloidomas) and pulmonary hypertension.1 It can be challenging to differentiate between pleural effusion caused by amyloid-induced cardiomyopathy and pulmonary amyloidosis. Treatment entails management of primary disease and in some cases pleural catheter placement. Our patient refused pleurodesis and opted for repeated thoracentesis.2
Bhandari BS, Gunjan R, and Jani P are responsible for the conception and design, acquisition of radiological data, drafting the article, critical revision of intellectual content and final approval of the version to be published.
FundingNone.
Conflicts of interestThe author declares that no conflicts of interest exist.