We present a 68-year-old patient with a history of former smoking and chronic B lymphocytic leukemia.
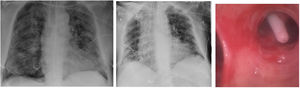
He was admitted in relation to bilateral pneumonia due to SARS-COV-2 infection and severe respiratory failure refractory to oxygen therapy. This worsening required him to be transferred to the Intensive Care Unit.1 After 26 days of admission, the patient developed a right pneumothorax (Fig. 1A) requiring an urgent chest tube drainage (pleurocath®, 8Fr, length 40cm, 2nd intercostal right space in the mid-clavicular line). Five days later, given that the right pneumothorax persisted, a new chest tube (equal measures and intercostal space) was inserted. Later, given the presence of persistent air leak, a fiberoptic bronchoscopy was performed to support the suspected diagnosis.2 This exploration revealed the presence of the pleural drainage's end placed at the entrance of 10th segment of the right lower lobe, confirming a bronchopleural fistula, as it is depicted in Fig. 1B and C. The catheters were removed and a 27F endothoracic tube was placed. The latter could be withdrawn after 7 days, then reaching a complete resolution of the pneumothorax and secondary bronchopleural fistula.
The authors state that they have no conflict of interests.