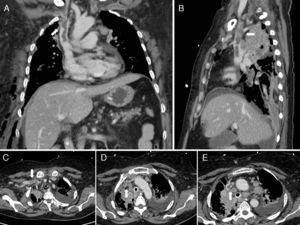
A 75-year-old woman with a history of diabetes presented with right shoulder pain and dyspnoea. Thorax CT scan showed a right pulmonary mass, bilateral pleural effusion and mediastinal adenopaties. Video-assisted thoracoscopic surgery with pleural sealing was performed. One hour after surgery, she suddenly presented dyspnoea and cyanosis, that extended from the upper thorax to her face, neck and both arms. The patient was intubated. Chest CT-scan showed a vena cava thrombosis (Fig. 1) and superior vena cava syndrome. Anticoagulation was started immediately, and the cyanosis resolved completely in 24h. The patient was weaned from mechanical ventilation, and discharged home.
Coronal (A) and sagittal (B) image of chest computed tomography showing the L-shape thrombus on right subclavian and superior cava vein (white arrow). Axial image of chest computed tomography (C) displaying the possible origin of the thrombus in the subclavian vein. Axial image of chest computed tomography (D and E) showing the venous thrombus going through the superior vena cava (white arrow).
Superior vena cava syndrome (SVCS) is not uncommon in patients with malignancy. However, acute development of this syndrome is rare1. It is a medical emergency that occurs due to extraluminal compression or acute intraluminal obstruction of the superior cava vein. Due to the L-shape of the lesion, we believe that the patient had a subclavian thrombosis secondary to malignancy-related hypercoagulability2 that migrated to the cava vein after the surgery, and this was responsible for the sudden onset of symptoms. Acute SVCS is a critical condition in which immediate diagnostic and therapy are imperative to avoid life-threatening complications.