The maximum standardised uptake value (SUVmax) is a widely utilised metric in positron emission tomography/computed tomography for clinically staging non–small-cell lung cancer (NSCLC), yet the reliability of SUVmax remains controversial. We herein aimed to assess the effectiveness of semi-quantitative parameters, encompassing size, SUVmax, metabolic tumour volume (MTV), total lesion glycolysis (TLG) and heterogeneity factor (HF), in evaluating both primary tumours and lymph nodes (LNs) on positron emission tomography/computed tomography. A novel scoring system was devised to appraise the role of semi-quantitative parameters and visually evaluate LNs for nodal staging.
Materials and MethodsPatients with pathological NSCLC, diagnosed between 2014 and 2019 and clinically staged I-III, were enrolled in the study. Patient demographics, including age, sex, tumour location, diameter, tumour-node-metastasis stage, as well as SUVmax, MTV, TLG and HF parameters of primary tumours and LNs, were documented.
ResultsThe analysis comprised 319 patients and 963 LNs. Patients had a mean age of 61.62 years, with 91.5% being male. Adenocarcinoma exhibited a histological association with LN metastasis (P=0.043). The study findings revealed that tumour size, SUVmax, MTV, TLG and HF did not significantly affect the detection of LN metastasis. Conversely, non-squamous cell carcinoma, LNs exhibiting higher FDG levels than the liver, LN size, SUVmax, MTV and TLG were identified as risk factors (P<0.0001). The identified cut-off values were 1.05cm for LN size, 4.055 for SUVmax, 1.805cm3 for MTV and 5.485 for TLG. The scoring system incorporated these parameters, and visual assessment indicated that a score of ≥3 increased the risk of metastasis by 14.33 times.
ConclusionWe devised a novel scoring system and demonstrated that LNs with a score of ≥3 in patients with NSCLC have a high likelihood of metastasis. This innovative scoring system can serve as a valuable tool to mitigate excessive and extreme measures in the assessment of invasive pathological staging.
Non–small-cell lung cancer (NSCLC) accounts for approximately 85% of all lung cancers, with up to 40% of patients with NSCLC exhibiting metastatic disease upon diagnosis.1 Accurate mediastinal staging is imperative for devising optimal treatment strategies and effectively managing patients. While invasive procedures serve as the gold standard for nodal staging, their utilisation is hampered by inherent risks of complications, cost concerns and diagnostic delays.2 Non-invasive mediastinal lymph node (LN) staging presents a promising alternative to identify patients requiring invasive interventions. Positron emission tomography/computed tomography (PET/CT) with 18F-fluorodeoxyglucose (18F-FDG) emerges as a non-invasive modality for cancer staging, restaging, radiotherapy planning and treatment response prediction.3,4
However, reliance solely on the maximum standardised uptake value (SUVmax) for quantifying metabolic activity in 18F-FDG PET/CT poses limitations. SUVmax provides a single voxel value that is insufficient for capturing the entirety of tumour volume or offering comprehensive insights into overall tumour metabolism. Consequently, it falls short as a determinant of the heterogeneous nature of lung tumours characterised by distinct biological activity regions.5 Moreover, guidelines caution against considering SUVmax of the primary tumour as a reliable biomarker for determining disease prognosis.6,7 Recent research underscores the potential of alternative parameters such as metabolic tumour volume (MTV), total lesion glycolysis (TLG) and heterogeneity factor (HF), derived from SUV calculations on PET/CT scans, as robust prognostic indicators.5,8–12 MTV reflects metabolically active tumour volume, while TLG signifies both volumetric and metabolic tumour burden, offering more nuanced measures of tumour aggressiveness and burden.13–16 Notably, intra-tumoural heterogeneity, quantified by the FDG uptake heterogeneity factor, emerges as a salient predictor of lymph node metastasis (LNM) across various malignancies.17–19 Leveraging semi-quantitative parameters of the primary tumour and LNs in F-18 FDG PET/CT, our study aims to discern their efficacy in predicting LNM during NSCLC clinical staging. Additionally, we analyse the utility of a novel scoring system incorporating these parameters alongside visual LN assessment for enhanced mediastinal staging accuracy.
MethodsPatient selectionThis retrospective analysis encompassed 319 patients and 963 LNs diagnosed with early and locally advanced NSCLC at the Atatürk Sanatorium Training and Research Hospital of the University of Health Sciences, Ankara, between January 2014 and December 2019. The hospital's computer system archives PET/CT scan images obtained before treatment, primary pathological lung cancer diagnoses, mediastinal LN pathological diagnoses obtained via endobronchial ultrasound (EBUS) and/or surgical methods (mediastinoscopy or operation) and clinical follow-up data. These data were retrieved from the system and file records. Patients with complete information available were included in the study. F-18 FDG PET/CT scans of patients with NSCLC retrievable from our hospital database were re-examined. Patients staged as I, II (early clinical stages) and III (locally advanced stage) according to the 8th tumour node metastasis staging system were included in the study.
The following patients were excluded: 1. Patients with indistinguishable primary tumour and LN involvement on PET/CT due to proximity and those receiving malignancy treatment between PET/CT and LN sampling; 2. Patients undergoing any malignancy treatment between PET/CT and LN sampling; 3. Stage III patients with scalene/supraclavicular LN metastases; 4. Patients with distant disease (stage 4) and, 5. Patients with unavailable results in the hospital database.
The research commenced upon obtaining approval from the Ethics Committee of the University of Health Sciences, Keçiören Training and Research Hospital, in accordance with guidelines (14.09.2021/2012-KAEK-15/2365).
LN samplingGiven the retrospective nature of the study, patients undergoing EBUS and/or surgical LN sampling were included. As per the European Society of Thoracic Surgeons20 and European Society for Medical Oncology21 guidelines, the diagnostic approach to NSCLC-suspected lesions is guided by clinical stage:
Mediastinal pathological staging is recommended for central tumours, suspected N1 disease and tumours >3cm. Additionally, younger age, adenocarcinoma (ADC) histology and higher N stage on PET/CT, N2 and N3 are deemed risk factors for the disease. For lesions suspicious of T1a-cN0M0 (stage I) with a peripheral location of <3cm or clinically mediastinal location and no suspicion of distant metastasis with hilar LN involvement, surgery is advised.20,21
A comparative investigation into the optimal number of LN stations necessitating sampling through the combined utilisation of endoscopic ultrasound (EUS) and EBUS for mediastinal staging remains unexplored. Nonetheless, established protocols related to mediastinoscopy, regarded as the gold standard for mediastinal staging, provide valuable insights. According to the 2014 guideline on mediastinal staging by the European Society of Thoracic Surgeons, the evaluation and sampling of at least stations 4L, 4R and 7 are recommended during cervical mediastinoscopy. Additionally, the guideline suggests the sampling of LNs 2R and 2L, if present, and LNs 5 and 6, which could potentially influence treatment strategies, particularly in cases of left-sided tumours. In the guide outlining the combined application of EBUS and EUS, it is advised to sample at least stations 4R, 4L and 7 for comprehensive mediastinal staging (EBUS+EUS). Moreover, the guidelines recommend sampling pathological LNs with PET/CT.20,21
Data collectionDemographic data, including age and sex, alongside pathological diagnoses of the primary tumour and LNs, were retrospectively analysed. Patients were stratified into subgroups of ADC, squamous cell carcinoma (SCC), adenosquamous cell carcinoma and not otherwise specified based on a review of pathological diagnoses of the primary tumour. The 8th tumour node metastasis staging system was applied for classification.22
FDG-PET/CT scan protocolPatients underwent FDG PET/CT imaging using a Siemens Biograph-6-HI-REZ integrated PET/CT scanner (Siemens Medical Solutions, Knoxville, Tennessee, USA). The imaging protocol entailed a 6-h fasting period before scanning, with patients encouraged to drink water. Following confirmation of acceptable peripheral blood glucose levels (<180mg/dL), patients received an intravenous injection of 370–555 MBq (10–15 mCi) FDG and underwent a 60-min rest before scanning. Initially, CT scans were conducted from the head to the thigh with the arms elevated, utilising the CareDose (Siemens) protocol. Subsequently, PET data acquisition entailed 3-minute scans per bed position, spanning 6–8 bed positions. CT data were utilised for attenuation correction, and PET images were reconstructed employing a Gaussian post-filtering algorithm with 4 iterations and 8 subsets.
2.5 F-18 FDG PET/CT image evaluationAll PET/CT scans of the enrolled patients were analysed by a certified nuclear medicine specialist. After image reconstruction, the SUVmax and SUVmean values were calculated by outlining the region of interest around the primary tumour in the PET/CT images (fig. 1). The size and location of the primary tumour, including right/left and central/peripheral, were documented (Fig. 1a). SUVmax was determined as the maximum SUV value of the region of interest using the following formula: tissue concentration (MBq/mL)/injected FDG activity (MBq)/body weight (g). MTV was defined as the volume of the tumour exceeding the SUV threshold of 2.5, while TLG was calculated by multiplying SUVmean and MTV. LNs exhibiting higher FDG uptake than the mediastinal blood pool was categorised as positive. In cases of multiple positive LNs within the same station, the study included the SUVmax value of the LN with the highest FDG uptake. The MTV of the LNs was calculated using a 2.5 SUV threshold value. In cases of multiple LNs within the same station, the MTV of all LNs was summed, and TLG was calculated by averaging the SUVmean values for the LNs within that station. Furthermore, subcategories were established through visual comparison of the FDG uptake in the LN against that in the mediastinum and liver.
1a. An example of measurement of primary tumor and lymph node metabolic parameters in 18F-FDG PET/CT imaging. Figure represents primary tumor and metastatic lymph node. Primary tumor SUVmax 15.63 and MTV 179.66 cm3; lymph node SUVmax 8.67 and MTV 6.94 cm3. 1b. An example of the heterogeneity factor calculations. The graph in the figure shows that HF is calculated by taking the derivative of the volume threshold function for each tumor. The absolute value of the calculated slope forms the HF value.
The MTV values were computed for primary tumours and LNs using SUVmax threshold values of 40%, 50%, 60%, 70% and 80%. To determine HF, the volume-threshold function derivative of the MTV values obtained from each tumour threshold value was calculated using linear regression (Fig. 1b). HF values below 40% and above 80% were excluded from the analysis, as prior studies indicated that values below 40% indicate excessive normal tissue background activity, and those above 80% are susceptible to small volume and partial volume effects.18,19,23 All calculations were performed using the Siemens automatic operating system.
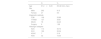
Development of a scoring systemWe identified statistically significant cut-off values for LN metabolic parameters potentially linked to LN metastasis. LNs meeting or exceeding the cut-off values for size, SUVmax, MTV and TLG, and exhibiting higher FDG uptake than the liver on visual comparison, were assigned with a score of 1. Nodes below the cut-off points or with lower FDG uptake than the liver were assigned with a score of 0 (Table 3). A 5-point scoring system was established, and the statistical robustness of this system was evaluated.
Cut-off values and diagnostic accuracy of LN size, SUVmax, MTV and TLG measurements in predicting LN metastasis.
| Area | p | 95% CI | Cut-off | Sens.% | PPV % | Spec. % | NPV % | OR | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||||
| Size | 0.795 | 0.0001 | 0.759 | 0.831 | 1.05 | 65.10 | 48.06 | 80.50 | 89.30 | 7.69 |
| SUVmax | 0.879 | 0.0001 | 0.848 | 0.909 | 4.055 | 80.90 | 53.8 | 80.80 | 93.84 | 17.75 |
| MTV | 0.849 | 0.0001 | 0.817 | 0.882 | 1.805 | 77.50 | 48.80 | 77.50 | 92.55 | 11.84 |
| TLG | 0.860 | 0.0001 | 0.828 | 0.892 | 5.485 | 78.0 | 49.54 | 78.0 | 92.74 | 12.76 |
SUVmax: maximum standardised uptake value; MTV: metabolic tumour volume; TLG: total lesion glycolysis; Sens: sensitivity; Spec: specificity; PPV: positive predictive value; NPV: negative predictive value; OR: odds ratio; CI: confidence interval.
Statistical analyses were conducted using IBM SPSS 25.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics were applied: continuous and discrete numerical variables were expressed as mean±standard deviation, while categorical variables were presented as counts and percentages. The Mann–Whitney U test was used for group comparisons, the chi-square method for analysing relationships between categorical data, and the Spearman correlation test for assessing variable relationships. Variables demonstrating statistical significance (P<0.05) in predicting LNM in univariate analysis were included in a multivariate logistic regression model. The diagnostic performance of independent risk factors (LN size, SUVmax, MTV and TLG) identified for predicting LNM in the multivariate analysis was evaluated through receiver operating characteristic (ROC) curve analysis. Threshold values were determined using the Youden index, and a scoring system was developed by ranking variables with independent risk factors. The scoring system's performance was assessed via ROC analysis, and diagnostic accuracy rates were calculated. A significance level of p<0.05 was used.
ResultsPatient characteristicsFrom January 2014 to December 2019, 2,240 patients with NSCLC underwent screening. Of these, 963 LNs from 319 patients meeting the inclusion criteria were included in this study (fig. 2). The median age of the cohort was 61.2±8.23 years (range: 25–82) years, with males accounting for 91.5% (n=292) (table 1). SCC was the most common primary histology, present in 52.04% of cases, followed by ADC at 35.74% (n=114). Among the 319 patients, 16.6% (n=53) were classified as stage I, 26.6% (n=85) as stage II and 56.7% (n=181) as stage III. The mean tumour size was 5.05±2.27cm, with the majority located centrally (67.7%, n=216) and on the right side (58.6%, n=187).
Characteristics of patients.
| N | % | |
|---|---|---|
| Age | 61.2±8.23 | 25–82 (min–max) |
| Sex | ||
| Male | 292 | 91.5 |
| Female | 27 | 8.5 |
| Diagnostic methods | ||
| FOB | 108 | 33.86 |
| TTNAB | 127 | 39.81 |
| EBUS | 78 | 24.45 |
| Surgery | 6 | 1.88 |
| Histologic subtypes | ||
| ADC | 114 | 35.74 |
| SCC | 166 | 52.04 |
| ADSC | 7 | 2.19 |
| NOS | 32 | 10.03 |
FOB: fiberoptic bronchoscopy; TTNAB: transthoracic fine needle aspiration biopsy; EBUS: endobronchial ultrasonography; ADC: adenocarcinoma; SCC: squamous cell carcinoma; ADSC: adenosquamous carcinoma; NOS: not otherwise specified; Min: minimum; Max: maximum.
Tumor size was measured in centimeters and categorized as T1, T2, T3, or T4, by the tumor, node, and metastasis (TNM) staging system. The T factor was taken from operated patients, whereas PET/CT measurements were taken from unoperated patients. The results showed that 21.6% (n=69) of patients were T1, 31.3% (n=100) were T2, 27.9% (n=89) were T3, and 19.1% (n=61) were T4. The number of patients with pN0 staging was 145 (45.4%), while the number of cN0 patients was 19 (5.96%). Of the patients, 109 (34.2%) were pN2 staged, while 119 (37.3%) were cN2 staged. The concordance between clinical and pathological N factors and stages was poor (κ=0.155, p<0.0001; κ=0.198, p<0.0001, respectively). A significant difference was observed in N factor and pathological staging according to cancer subtypes (p=0.002; p=0.01, respectively). Among SCC patients, 54.8% (n=91) were N0, while 43% (n=49) of ADC patients exhibited N2 disease. ADC accounted for 44.4% (n=12) of pN3 lymph nodes. A total of 64.9% (n=74) of ADC patients were diagnosed at stage III. Most patients diagnosed at an early stage (stages I-II) were diagnosed with SCC (p=0.01). Of the central tumours, 61.6% (n=133) were diagnosed as SCC, while 50.5% of peripheral tumours were diagnosed as ADC. In contrast to ADC, where the distribution of central and peripheral tumours was comparable, a significantly higher proportion of SCC cases (80.1%) were observed in the central region (p=0.0001).
PET/CT characteristics of primary tumour and LNsIn our study, the PET/CT findings for primary tumours were as follows: mean SUVmax 15.79±15.21, MTV 86.56±100.03, TLG 612.78±754.09 and HF 0.84±0.95. Although no statistically significant difference was observed, SUVmax, MTV, TLG and HF measurements showed higher values in tumours without LNM than in those with LNM (P>0.05). No correlation was found between tumour SUVmax and pathological staging (P=0.09); however, significant positive correlations were observed between tumour size (P<0.001, r=0.449), MTV (P<0.001, r=0.415), TLG (P<0.001, r=0.380), HF (P<0.001, r=0.432) and pathological staging.
The average time between PET/CT imaging and lymph node sampling was 18.02±15.72 days. A total of 963 LNs were analysed in our study, of which 209 (21.7%, n=209) showed metastasis. The LNs had a mean size of 1.01±0.52cm, SUVmax of 4.49±3.62, MTV of 3.64±8.62 and TLG of 17.07±50.95. Our results demonstrated a positive correlation between the size of the LNs and SUVmax, MTV and TLG (r=0.635, r=0.657, r=0.662, P<0.0001, respectively). Comparison between metastatic and non-metastatic LNs with LN size, SUVmax, MTV and TLG values showed that the measured metabolic parameters were significantly higher in patients with LNM than in those without LNM (P=0.0001). A visual comparison of 958 LNs with FDG uptake and liver and mediastinal blood pool activity (MBPS) showed that LNs with visually high FDG uptake from MBPS and liver had significantly more metastases (P<0.001). The sensitivity, specificity, negative and positive predictive values of PET-CT in detecting lymph node metastasis were 95.7%, 43.5%, 97.3%, and 31.9%, respectively.
Univariate and multivariate regression analyses results in predicting LN metastasisMultivariate logistic regression analysis was used to assess the variables associated with LNM in univariate analyses. Our results suggest that LNs with higher uptake than MBPS and ADC histology are not risk factors for LNM (P=0.434; P=0.086, respectively). Conversely, LN size, SUVmax, TLG, MTV, high liver FDG uptake and non-SCC histology are independent risk factors for predicting LNM. The results of univariate and multivariate regression analyses for predicting LN metastasis are shown in Table 2.
Results of univariate and multivariate logistic regression analyses in predicting LN metastasis.
| Univariate | Multivariate | |||
|---|---|---|---|---|
| Variables | OR (95% CI) | p-value | OR (95% CI) | p-value |
| LN>MBPS | 15.460 (10.126–23.603) | 0.001 | - | 0.434 |
| LN>L | 17.001 (8.584–33.670) | 0.001 | 1.933 (1.029–3.630) | 0.048 |
| SUVmax | 17.828 (12.071–26.331) | 0.001 | 3.108 (1.584–6.096) | 0.001 |
| MTV | 1.341 (1.275–1.410) | 0.001 | 1.067 (0.293–3.891) | 0.014 |
| TLG | 1.074 (1.060–1.087) | 0.001 | 1.080 (1.037–1.123) | 0.001 |
| Size | 12.951 (8.558–19.599) | 0.001 | 1.281 (0.689–2.383) | 0.005 |
| Non-SCC histology | 0.497 (0.363–0.681) | 0.001 | 5.113 (2.527–10.345) | 0.001 |
| ADC | 1.483 (1.241–1.971) | 0.041 | - | 0.086 |
SUVmax: maximum standardised uptake value; MTV: metabolic tumour volume; TLG: total lesion glycolysis; LN: lymph node; L: liver; MBPS: mediastinal blood pool activity; SCC: squamous cell carcinoma; ADC: adenocarcinoma; OR: odds ratio; CI: confidence interval.
ROC analysis curves for the prediction of LN metastasis are presented in Fig. 2a. The area under the curve (AUC) values were 0.795, 0.879, 0.849 and 0.860 for LN size, SUVmax, MTV and TLG, respectively (Table 3). Among the PET parameters, LN SUVmax exhibited the best predictive performance for LNM, with an optimal cut-off value of 4.055 (sensitivity 80.9%, specificity 80.8%).
Values above the defined threshold for LN size, SUVmax, MTV and TLG, as well as those with LN FDG uptake greater than that of the liver, were scored 1. Values below the threshold and LN FDG uptake less than that of the liver were scored 0. We developed a 5-point scoring system (table 4). A total of 958 LNs were scored, with 466 receiving a score of 0 and 186 receiving a score of 5. LNM was detected in 68.82% (n=128) of nodes graded with a score of 5. In comparison, 10.58% of metastatic nodes were scored 0 and 61.54% received a score of 5. Using ROC analysis, a cut-off value of 2.5 points was ascertained for these nodes (Fig. 3b). A score greater than 2.5 was associated with a 14.33-fold increased risk of LNM. Table 5 shows the sensitivity, specificity, positive and negative predictive values and odds ratios.
Distribution of data included in the scoring system.
| pN+N (%) | pN− N (%) | TotalN (%) | Point | ||
|---|---|---|---|---|---|
| LN size (cm) | >1.05 | 136 (14.19) | 145 (15.14) | 281 | 1 |
| ≤1.05 | 72 (7.52) | 605 (63.15) | 677 | 0 | |
| LN SUVmax | >4.055 | 168 (17.54) | 143 (14.92) | 311 | 1 |
| ≤4.055 | 40 (4.18) | 607 (63.36) | 647 | 0 | |
| LN MTV (cm3) | >1.805 | 162 (16.91) | 168 (17.54) | 330 | 1 |
| ≤1.805 | 46 (4.80) | 582 (60.75) | 628 | 0 | |
| LN TLG | >5.485 | 163 (17.01) | 164 (17.12) | 327 | 1 |
| ≤5.485 | 45 (4.70) | 586 (61.17) | 631 | 0 | |
| LN>L | 179 (18.68) | 214 (22.34) | 393 | 1 | |
| LN ≤ L | 29 (3.03) | 536 (55.95) | 565 | 0 | |
| Score | Total score: 5 | ||||
| 0 point | 22 (10.58) | 444 (59.2) | 466 (48.64) | ||
| 1 point | 12 (5.77) | 100 (13.33) | 112 (11.69) | ||
| 2 point | 12 (5.77) | 58 (7.73) | 70 (7.31) | ||
| 3 point | 4 (1.92) | 32 (4.27) | 36 (3.75) | ||
| 4 point | 30 (14.42) | 58 (7.73) | 88 (9.19) | ||
| 5 point | 128 (61.54) | 58 (7.73) | 186 (19.42) | ||
| 0–2 points | 46 (22.12) | 602 (80.3) | 648 (67.64) | ||
| 3–5 points | 162 (77.88) | 148 (19.7) | 310 (32.36) | ||
SUVmax: maximum standardised uptake value; MTV: metabolic tumour volume; TLG: total lesion glycolysis; L: liver; LN: lymph node.
Analysis of the scoring system for predicting LN metastasis.
| Presence of LNM | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| p | 95% CI | |||||||||
| Area | Lower | Upper | Cut-Off | Sens | PPV | Spec | NPV | OR | ||
| Score | 0.848 | 0.0001 | 0.816 | 0.880 | 2.5 | 77.9% | 52.23% | 80.3% | 92.9% | 14.33 |
PPV: positive predictive value; NPV: negative predictive value; OR: odds ratio; Sens: sensitivity; Spec: specificity; CI: confidence interval; LN: lymph node; LNM: lymph node metastasis.
This study delved into the efficacy of various semi-quantitative parameters, such as LN size, SUVmax, MTV and TLG, in predicting mediastinal LN metastasis. Additionally, we explored how these parameters, combined with primary tumour characteristics, including size, SUVmax, MTV, TLG, and HF, measured via 18F-FDG PET/CT, contribute to predictive accuracy. Our research suggests that a scoring system that integrates lymph node size, SUVmax, MTV, TLG and visual comparison is more effective in non-invasively staging lymph nodes for detecting positivity than relying on these parameters individually. Additionally, our study boasts the largest sample size to date for evaluating lymph node parameters.
Approximately 60%–70% of lung cancer diagnoses occur in individuals aged 65 or older, with men exhibiting a higher incidence. Notably, Lu et al. comprehensive analysis spanning 1973 to 2015 revealed a declining incidence of lung cancer in men, decreasing with a rising trend in women. Furthermore, their study highlighted a higher 5-year survival rate among women. Consistent with prevailing trends, our study predominantly comprised male participants (91.5%, n=292), with an average age at diagnosis of 61.62±8.23 years.
Age and tumour size serve as well-established risk factors for LNM in NSCLC.24 For instance, investigation of Kong et al. on patients with resected adenocarcinoma in situ (adenosquamous cell carcinoma) revealed a heightened likelihood of LNM among individuals younger than 65 years with tumours larger than 3cm in size.25 Intriguingly, neither sex nor histological subtype significantly influenced LNM likelihood, with optimal cut-off points identified at 64.5 years and 2.85cm for age and tumour size, respectively (AUC: 0.567, 95% CI: 0.544-0.591; AUC: 0.677, 95% CI: 0.656-0.698, respectively). Similarly, in a study focusing on peripheral early-stage lung ADC, tumour size emerged as a robust predictor of LNM, while age and sex exhibited negligible impact.26 However, our study did not unveil any significant associations between age, sex, tumour size and LNM (P=0.4, P=0.607, P=0.62). Notably, Miao et al. reported analogous findings, underscoring the non-predictive nature of age, sex and tumour size in patients operated for lung ADC.27 It is crucial to acknowledge the inherent heterogeneity within NSCLC subtypes, which may contribute to divergent prognostic outcomes across studies. The discrepancies observed in study outcomes may be attributed to heterogeneity.
LNM stands out as a key marker of malignancy, often indicating highly invasive tumours with poor prognoses.28 While invasive methods are typically preferred for mediastinal LN staging, there are situations, such as in patients with significant comorbidities, where invasive procedures may not be viable. In such cases, treatment decisions can be guided by a PET/CT-based clinical staging approach.29,30 In our study, the development of a scoring system based on predefined PET/CT parameters revealed a substantial 14-fold increase in the risk of metastasis in LNs scoring 3 and above.
Despite its widespread use, SUVmax, as a single parameter, has been found to be an unreliable indicator and inadequate for predicting prognosis, as highlighted in several studies.6,7,31,32 Relying solely on SUVmax for PET/CT interpretation can lead to the overlooking of LNM, with reported incidence rates varying between 8% and 58%.33 In another study, the false positive rate of PET-CT was found to be 25% (57 of 234 patients). Upon further analysis, the researchers determined that the histological subtype (squamous cell carcinoma) was the primary reason for this discrepancy.34 Recognising these limitations, recent research has focused on alternative methods for predicting metastasis. Volumetric parameters such as MTV, TLG and HF in PET/CT imaging have emerged as promising predictors and prognostic markers for LNM and staging across various cancer types. Clear and concise imaging metrics could significantly enhance cancer diagnosis and management.8,11,12,14,15,18,35 Our study revealed no association between the semi-quantitative parameters of the primary tumour and LNM. Although increased values for tumour size, MTV, TLG and HF were linked to advanced stage, they did not correlate with primary tumour SUVmax. These findings underscore the limited reliability of SUVmax as a parameter. However, they do suggest the potential suitability of other parameters as prognostic indicators, a notion supported by the study of Ouyang et al.17 In their analysis, tumour SUVmax and SUVmean values for ADC and SCC were not significant factors for LNM. Nevertheless, primary tumour MTV emerged as a crucial predictive factor, with an optimal cut-off value of 29.50 (AUC: 0.659, sensitivity: 70.4%, specificity: 59.2%) for occult LNM in patients with stage I ADC (P=0.044; OR: 1.671, 95% CI: 1.013-2.756). Similarly, an optimal cut-off value of 0.198 (AUC: 0.759, sensitivity: 88.9%, specificity: 61.1%) for primary tumour HF in patients with SCC was identified as an independent risk factor (P=0.023; OR: 8.799, 95% CI: 1.351–57.317).
In the mediastinal region, LNs with a short axis diameter greater than 10mm are commonly diagnosed as malignant on contrast-enhanced CT36; however, their sensitivity is relatively low at 59%, with a specificity of 78%.37 On the other hand, PET/CT imaging demonstrates a higher sensitivity (85%) in LNs larger than 1cm in diameter, dropping to 32% in smaller nodes.38 Kuzucuoglu et al. found that LNs with high FDG uptake, a size greater than 16mm and an SUVmax greater than 2.9 have a higher risk of metastasis.39 However, assessing LN metabolic and volumetric parameters for metastasis prediction is relatively uncommon compared with tumour evaluations. In a separate study, the SUVmax values of metastatic LNs were notably higher than in non-metastatic ones when considering SUVmax of ≥4 as PET-positive for metastasis.40 In this study, a correlation was found between tumour SUVmax, histological subtype and tumour size, with no such correlation found for LN SUVmax. Studies have established an SUVmax threshold of ≥2.5 as appropriate for detecting pathological LNs.41 A meta-analysis suggested that for the mediastinal staging of NSCLC, PET/CT based on the SUVmax ≥2.5 positivity criterion has a sensitivity of 81% and specificity of 79.4%, while based on LN FDG uptake higher than the background activity criterion, the sensitivity and specificity estimates were 77% and 90%, respectively.4
In a 2016 study, Rogasch et al. demonstrated that LNs with visual FDG uptake higher than that of the liver (LN>L) were 3.3 times more effective in detecting malignancy than LN with lower uptake than the liver but with more MBPS (LN>MBP).42 This study involved 86 patients with NSCLC, with three experts of varying experience levels analysing the PET images. Their evaluations produced comparable results, indicating the reproducibility of the suggested classification. In a related recent study with a larger patient sample, it was noted that LNs with higher uptake from the liver (LN>LBC) necessitate less invasive staging than those with higher MBPS (LN>MBPS).43 However, while a lower false-positive rate would be achieved, there is a risk of missing more N2 diseases, including multiple diseases. Therefore, to mitigate excessive invasiveness in staging, the authors proposed limiting invasive staging to patients with all three risk factors (cN1, tumours larger than 3cm and central tumours), in line with existing guideline recommendations.20,21
In our study, we observed a 1,933-fold visual increase in the risk of LNM with high FDG uptake from the liver. Our results showed that 44.3% (n=424) of LNs were oversampled because high FDG uptake corresponding to the mediastinal blood pool (LN>MBPS) was considered positive for PET. If LNs with a higher FDG uptake than the liver (LN>L) had been considered positive, this figure would have been 22.3%. Notably, our scoring system achieved the lowest number of unnecessary invasive procedures, with a rate of 15.1%.
There is a noticeable gap in the current literature regarding LN metabolic parameters, leading to uncertainty about their clinical utility. While LN SUVmax, MTV and TLG have been linked to recurrence,44 volumetric parameters (MTV and TLG) have been reported to carry a higher prognostic risk than metabolic parameters (SUVmax and SUVmean). A recent study by Nakanishi et al. explored LN SUVmax, MTV, TLG and LPR (LN/primary tumour SUVmax) in 84 pN+ patients, revealing significantly higher values in metastatic LNs than in benign ones.45 The authors established cut-off values for LN SUVmax and TLG as 4.15 (sensitivity: 79.4%, specificity: 76.2%) and 1.26 (sensitivity: 81%, specificity: 76.2%), respectively. However, MTV, TLG and SUVmax did not emerge as independent risk factors for predicting metastasis. To the best of our knowledge, this investigation was the primary one to examine metabolic parameters in the LN, wherein the authors used an SUVmax cut-off value of 3.5 for calculating MTV and TLG, highlighting potential limitations due to sample size inadequacy.
In a study by Hua et al., which analysed 206 LNs, parameters such as LN size, SUVmax, SUVmean and TLG were found to be higher in metastatic LNs than in non-metastatic ones (P<0.001). However, MTV was higher in non-metastatic LNs, although not statistically significant.46 The study identified optimal diagnostic cut-off values as 5.47 for SUVmax, 10.30 for TLG and 9.90mm for LN size. Both studies suggest that LN TLG is elevated in metastatic LNs, but differences in results between studies underscore the lack of standardisation in calculating MTV. In our investigation, TLG emerged as a distinct risk factor for LN metastasis, particularly when the SUV cut-off was set at 2.5. If semi-quantitative parameters continue to offer reliable predictions of LN metastasis, the development of an automated system utilising a validated method could enhance clinicians’ ability to assess metastatic potential based on routine PET values.
In our study, we identified semi-quantitative measures of LNs and non-squamous histology as independent risk factors for LNM. Our novel scoring system represents a simple and promising approach for treatment planning and monitoring in patients with early and locally advanced NSCLC who are ineligible for invasive staging due to contraindications, refuse surgery, or when traditional methods fail to provide a definitive diagnosis.
It is important to note that this scoring system not only aids in avoiding unnecessary invasive procedures but also ensures prompt initiation of treatment, thus potentially reducing the economic burden on healthcare systems by avoiding unnecessary resource utilisation. Additionally, reducing the time between diagnosis and treatment of lung cancer can lead to better patient outcomes. Overall, we believe that implementing this scoring system could significantly reduce the cost of managing lung cancer while improving patient care.
LimitationsNonetheless, our study has several limitations. First, its single-centre design constrained the sample size. Second, the retrospective nature of the study meant that not all LNs with heightened uptake on PET/CT were sampled. Moreover, the inclusion criteria focused solely on patients undergoing EBUS for staging, potentially overlooking other cases. Furthermore, LNs evaluated with EBUS exhibiting sonographically benign criteria were not histopathologically evaluated, potentially introducing bias. A prospective study design, especially categorising cancer subtypes separately, could yield more robust results. Additionally, the lack of standardisation in the 18F-FDG PET/CT imaging protocol for measuring MTV and TLG poses a challenge. The segmentation method for determining MTV is still evolving, and there is currently no validated technique. Variability in studies arises from calculations using different SUV threshold values. Moreover, the fixed threshold SUV of 2.5 used to calculate MTV and TLG may lead to overestimation in tumours with high FDG uptake and underestimation in those with low uptake due to the exclusion of areas below the threshold value.
ConclusionThe developed scoring system aims to predict the likelihood of LNM in malignancies and to reduce unnecessary invasive staging. Our research identifies high FDG uptake in LNs from the liver, along with LN size, SUVmax, MTV and TLG, as independent risk factors for LNM. These parameters offer supplementary advantages to current clinical staging methods, potentially decreasing the need for invasive procedures. For individuals with a total score below 2.5, invasive staging may not be warranted. LNs scoring 3 or above exhibit a high likelihood of metastasis, indicating their suitability for invasive pathological staging. However, multi-centre studies with larger patient cohorts are necessary to validate this scoring system before routine implementation. Furthermore, this scoring system could be applied not only for LNM but also for the differential diagnosis of various LN conditions, such as granulomatous, reactive, or anthracotic LNs. Future studies on a larger scale are imperative to comprehensively validate this approach.
Declaration of Congress AbstractThis study has not been published or presented any where before.
EthicIn this study, national and international ethical rules are observed.
Ethic BoardEthics Committee of the University of Health Sciences, Keçiören Training and Research Hospital (14.09.2021/2012-KAEK-15/2365).
Financial DisclosureThe authors declared that this study has received no financial support.
Authors’ ContributionsAyperi Öztürk and Özlem Özmen: conceptualization, methodology, software. Özlem Özdağ: data curation, writing- original draft preparation. Ebru Tatcı and Figen Öztürk Ergür: visualization, investigation. Özlem Özmen: supervision, validation. Figen Öztürk Ergür: writing. Aydın Yılmaz and Ayperi Öztürk: reviewing and editing.
Conflict of InterestNo conflict of interest was declared by the authors.