Vanishing lung syndrome is a rare condition characterized by unilateral or bilateral asymmetric upper lobe involvement with the formation of multiple large bullae replacing normal pulmonary architecture and compressing surrounding parenchyma.1
In this paper, we report the case of a male cystic fibrosis (CF) patient with severe sinopulmonary disease, malnutrition, diabetes mellitus and asthenozoospermia. He was diagnosed with CF at 3 years of age due to malnutrition and recurrent respiratory infections. His sweat chloride concentration was 101mmol/L and CFTR gene mutations were F508del and 2935del11. At the age of 30, he was evaluated for a lung transplant and chest imaging studies were performed, see Fig. 1. Previous chest X-rays had showed slowly progressing changes in the upper areas of both lung fields over the past 3 years.
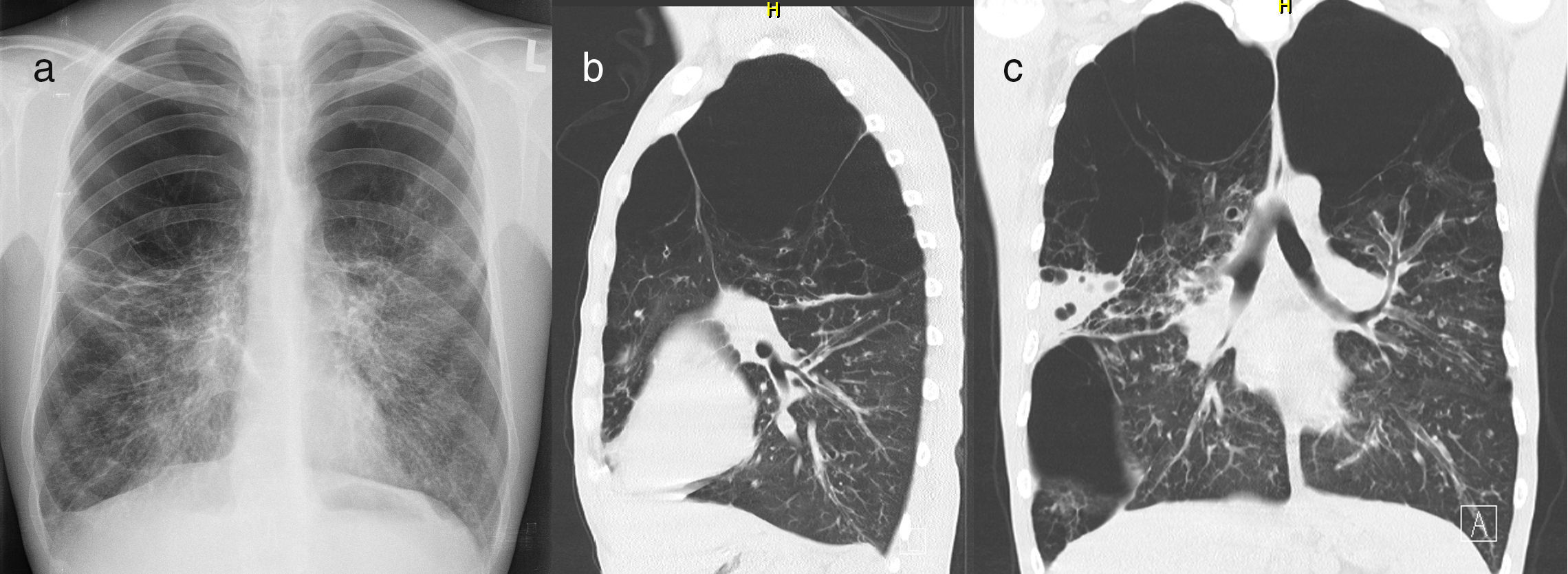
Chest X-ray and chest CT. (a) Posteroanterior chest X-ray shows hyperlucent upper parts of both lung fields, approx. upper half on the right side and upper third on the left side. Residual lung parenchyma has increased bronchovascular markings; (b) Chest CT (sagittal reconstruction) at the level of left hilum shows vanishing lung in the upper third of left lung; (c) Chest CT (coronal reconstruction) at the level of main bronchi shows bronchiectasis in the left upper lobe ending in severe emphysematous changes of lung parenchyma, vanishing lung in both upper zones, large bulla in the right lower lobe and consolidation in basolateral part of the right upper lobe.
In patients with CF, the typical CT picture is bronchiectasis, bronchial wall thickening, mucus plugging, atelectasis, consolidation and air trapping.2 Emphysematous and bullous changes are not consistent with CF lung disease. Our patient was a never-smoker and had normal levels of serum α1-antitrypsin, with no symptoms of other diseases that may be complicated by vanishing lung syndrome or giant bullae (e.g. sarcoidosis, granulomatosis with polyangiitis or Marfan and Ehlers–Danlos syndromes).