We read with interest the editorial published in your journal on the usefulness of diaphragmatic ultrasound (DUS).1 We would like to mention another use for DUS in addition to those proposed by the authors1: the preoperative evaluation (PE) of patients scheduled to undergo cardiovascular surgery. Measuring the diaphragmatic shortening fraction (DSF) in the preoperative period can help detect patients at increased risk of postoperative complications.2 A DSF of less than 20% is considered low and confers a high risk. Normal DSF is 36% to 38%, and a DSF of less than 38% is associated with postoperative complications.2,3 A reduction in DSF of more than 10% measured 1 day after surgery has also been associated with postoperative complications such as prolonged stay in the intensive care unit.2,3
We report the case of a 78-year-old man with diabetes mellitus, kidney failure, active smoking, and mild malnutrition who was scheduled for elective cardiovascular surgery for myocardial revascularization. In the PE, the patient had a NYHA functional class II and ASA score of II.4 Pulmonary and cardiovascular physical examinations were normal. Spirometry was normal and oxygen saturation was 94%.
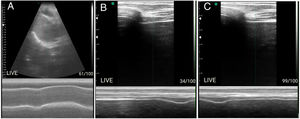
We measured the DSF of the right diaphragm in the zone of apposition using a portable multifrequency linear transducer that was placed longitudinally on the right anterior axillary line between the seventh and eighth intercostal space.5 DSF was 40%, so we were confident that the risk of complications would be very low (Fig. 1). While the patient's characteristics did not suggest a particularly high risk, the clinical evaluation performed with predictive scales for postoperative complications indicated a moderate risk (6.6%) of myocardial infarction, pulmonary edema, ventricular fibrillation, and cardiac arrest, and a very high risk (42.1%) of perioperative pulmonary complications according to the ARISCAT scale,4 the clinical scale that we routinely use for PE. A very high risk on the ARISCAT scale prompts us to perform other pre-surgery evaluations; however, in this case the decision was made on the basis of the DSF. This finding was reported to the cardiovascular surgeon and the decision was made to schedule surgery. DSF 24h after surgery was 38%.2 The patient had no immediate cardiopulmonary complications, was extubated early, left the intensive care unit on the third day, and showed very good postoperative progress.
(A) Diaphragmatic dome in 2D and anatomical M modes with convex transducer showing displacement of the dome in vital capacity. (B) Diaphragm in zone of apposition with linear transducer and measurement of thickness in maximum expiration. (C) Diaphragm in zone of apposition with linear transducer and measurement of thickness in minimum expiration. (B and C) For calculation of preoperative shortening fraction.
We share the authors’ view that DUS, with all its advantages, has become one of the best tools in the pulmonologist's diagnostic arsenal,1 thanks to its non-invasive nature, low cost, wide availability, use at the bedside, absence of adverse effects, and acceptable reproducibility. It has very few disadvantages, and is an excellent addition to the clinical PE of patients with a high risk of complications estimated by ARISCAT.
FundingThe authors declare that they have not received funding for this work.
Please cite this article as: Pecho-Silva S, Navarro-Solsol AC. Utilidad de la ecografía diafragmática en la evaluación preoperatoria. Arch Bronconeumol. 2020;56:764–765.