Extracorporeal carbon dioxide removal (ECCO2R) is an advanced form of life support that is mostly used in patients with acute respiratory distress syndrome (ARDS) and severe acute exacerbations of chronic obstructive pulmonary disease (COPD) or asthma.1,2 For the former, ECCO2R therapy allows ultra-protective lung ventilation and reduces ventilator-induced lung injury. For the latter, ECCO2R therapy may be applied to prevent intubation in patients at risk of non-invasive ventilation (NIV) failure.3,4 Due to the need for venous cannulation and complexity of care, this technique is mainly used in Intensive Care Units (ICU).5 We present a case of successful treatment with a peristaltic pump ECCO2R in an Intermediate Respiratory Care Unit (IRCU).
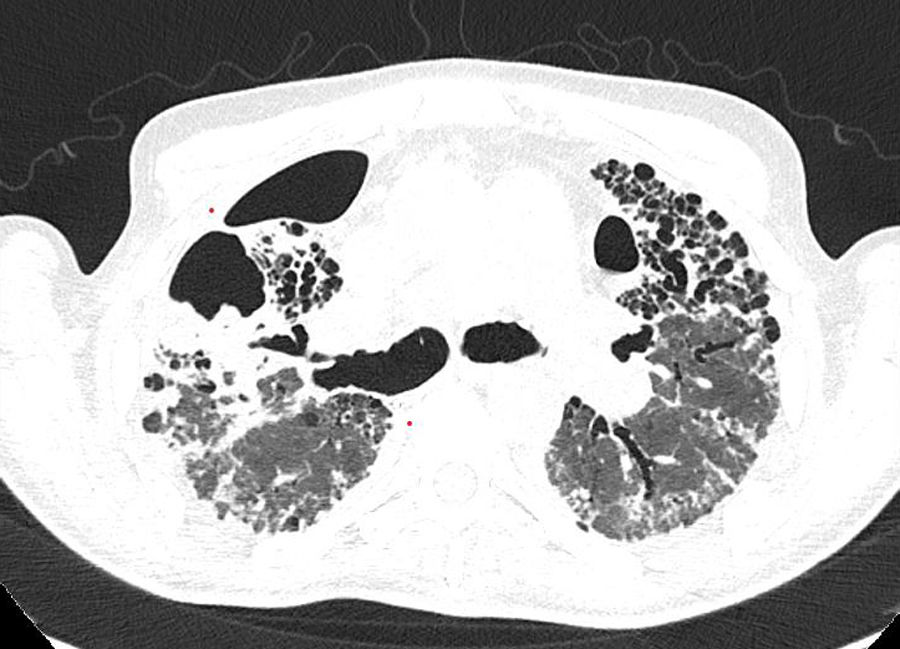
A 67-year-old male with a history of progressive pulmonary fibrosis after COVID-19 (Fig. 1), referred for evaluation for lung transplant at last pneumology follow-up, was admitted to the hospital because of severe respiratory insufficiency. His medical record included chronic lymphocytic leukaemia (in remission), pulmonary embolism and atrial fibrillation on anticoagulation. He presented with a recent onset of dyspnoea, cough with purulent sputum, fever and increased oxygen requirement. Blood pressure was 122/65mmHg, pulse 100bpm, SaO2/FiO2 112, and a respiratory rate of 40bpm with scattered bilateral crackles. Blood gases showed respiratory acidosis (pH 7.27, pCO2 116mmHg, pO2 38mmHg, HCO3 53.3mM/L). A chest X-ray revealed a known interstitial pulmonary infiltrate without significant changes compared to his previous one. Laboratory studies showed an increased C-reactive protein (136.0mg/L), leukocytosis (14.70×10^3/μl), and neutrophilia (10.90×10^3/μl). Since the patient had a do-not-intubate order, he was admitted to the IRCU.
NIV was started but, after 24h, the condition of the patient did not improve. Faced with this situation of non-invasive measures failure in a patient pending evaluation for lung transplant with a potentially reversible acute worsening due to an infectious disease as the most likely cause, the patient was connected to an ECCO2R device (Prismalung+, Baxter) and empirical antibiotic treatment was started. Blood flow was kept between 250 and 300ml/min and gas flow (oxygen) at 6–8L/min, which was well tolerated by the patient, being able to withdraw NIV and deescalate to high-flow and finally conventional nasal cannulas. At the beginning of treatment ABG showed pH 7.4, pCO2 93mmHg, pO2 88mmHg and HCO3 57.6mM/L (PaO2/FiO2 110), with persisting tachypnea (40bpm) and work of breathing. After 24h, ABG improved to pH 7.43, pCO2 60mmHg, pO2 54mmHg, HCO3 39.8mmHg with respiratory rate around 20bpm, PaO2/FiO2 135 and no dyspnoea. As the patient's clinical condition improved following medical treatment, it was possible to withdraw ECCO2R after 6 days and the patient was discharged home.
The use of ECCO2R has been reported in the ICU setting. This case represents the potential use of ECCO2R in an IRCU in reversible situations refractory to non-invasive measures. Further research is required to determine the best way to implement this therapy in IRCU, to maximize its benefits while minimizing any potential risks.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestEsther Barbero Ph.D. None.
Antonio Gomis M.D. Has received lectures honoraria from Baxter International Inc., Deerfield, Illinois.
David Pestaña Ph.D. Has received honoraria from Baxter International Inc. Baxter International Inc., Deerfield, Illinois; and B. Braun Medical S.A.
Artificial intelligence involvementHelp of any artificial intelligence software or tool has not been use for this publication.