Floppy epiglottis is a type of laryngomalacia rarely seen in clinical practice. In these patients, epiglottal collapse causes a mechanical alteration that may lead to airflow obstruction associated with symptoms of stridor, dyspnea, and respiratory failure. These symptoms are similar to those found in laryngeal obstruction caused by asthma, vocal cord paralysis, tumors, or foreign bodies, among others, and are sometimes difficult to diagnose.1 We report the case of a patient who was diagnosed with floppy epiglottis during awake orotracheal intubation (OTI) with C-MAC videolaryngoscope (VL) for respiratory failure due to upper airway obstruction.
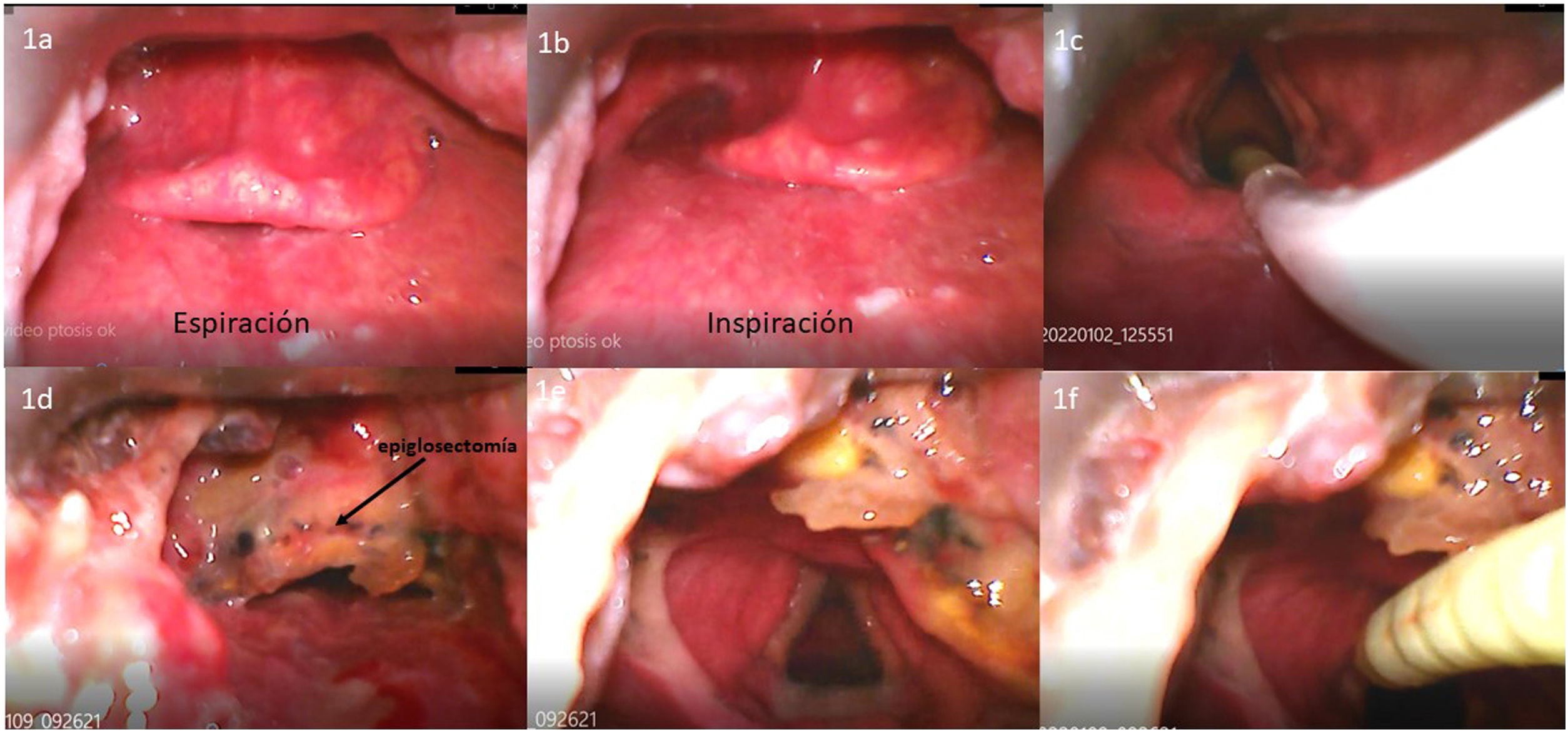
This was a 76-year-old patient with a history of sleep apnea who underwent laparoscopic Ivor Lewis esophagectomy for esophageal cancer. In the immediate postoperative period, the patient presented respiratory distress with stridor, requiring OTI. During his stay in the intensive care unit, the patient was extubated and 2 further attempts at intubation were made due to a similar clinical picture of respiratory failure with stridor. After extubation, the patient did not respond to either high-flow oxygen therapy or non-invasive mechanical ventilation (BIPAP: 25cm H2O IPAP and 7cm H2O EPAP). Following a third episode of respiratory distress, we decided to intubate the patient while awake, using C-MAC VL (KARL STORZ Germany 8403HX) in an attempt to diagnose the cause of the obstruction. Topical anesthesia was administered with 10% lidocaine aerosol and a transtracheal injection of 2mL of 4% lidocaine. VL revealed a large, flaccid epiglottis that totally obstructed the view of the glottis (Fig. 1a) and prolapsed into the glottis during inspiration, obstructing airflow (Fig. 1b). An adequate view of the glottis was obtained by lifting the epiglottis with the VL blade, so we decided to perform OTI guided by a flexible-tipped bougie (Fig. 1c). After the diagnosis, epiglottectomy was performed, but the patient's clinical picture remained unchanged. C-MAC VL showed how the remaining epiglottis prolapsed toward the glottis during inspiration, causing airflow obstruction (Fig. 1d). The patient was reintubated under spontaneous breathing using a flexible-tipped bougie guided by C-MAC VL (Fig. 1e and f). Given the difficulty in managing the patient's airway, definitive surgical tracheostomy was performed.
C-MAC videolaryngoscopic view in spontaneous breathing showing a floppy epiglottis preventing visualization of the glottis ((a) inspiration and (b) expiration). The epiglottis was lifted with the videolaryngoscope blade, allowing full visualization of the glottis. In spontaneous breathing, a flexible-tipped bougie was inserted and OTI could be performed (c). After the epiglottectomy, laryngoscopy showed how the remaining epiglottis prevented visualization and prolapsed slightly toward the glottis on inspiration (d). The epiglottectomy area was lifted with the videolaryngoscope blade, permitting the visualization of the glottis (e), and a flexible-tipped bougie was inserted through the glottis for patient intubation (f).
The use of awake VL for OTI in patients with difficult airway predictors provides a wide-angle view of the oral cavity and its structures, and can aid in the diagnosis of various upper airway diseases.2–5 Furthermore, due to its rigidity, the VL blade can be used to lift masses or structures that compromise airway access, as in our case, in which we lifted the floppy epiglottis that obstructed the entrance to the glottis, thus facilitating OTI.
FundingNone declared.
Authors’ contributions- -
Conceptualization: Manuel Taboada, Javier Segurola, Javier García, Laura Dos Santos.
- -
Data collection: Javier Segurola, Javier García.
- -
Writing – original draft preparation: All authors helped revise the draft of the manuscript.
- -
Writing – review and editing: All authors.
The authors have no conflict of interests.
The authors would like to thank their colleagues in the critical care unit.