To the Editor:
Although silicosis is a very ancient disease, new cases are still reported (in Spain more than 200 new cases are diagnosed ever year).1 Given that silica is present almost everywhere, apart from in professions in which there is known to be exposure to this dust, silicosis reports continue appearing from industries and work environments that were no previously recognised as a risk.
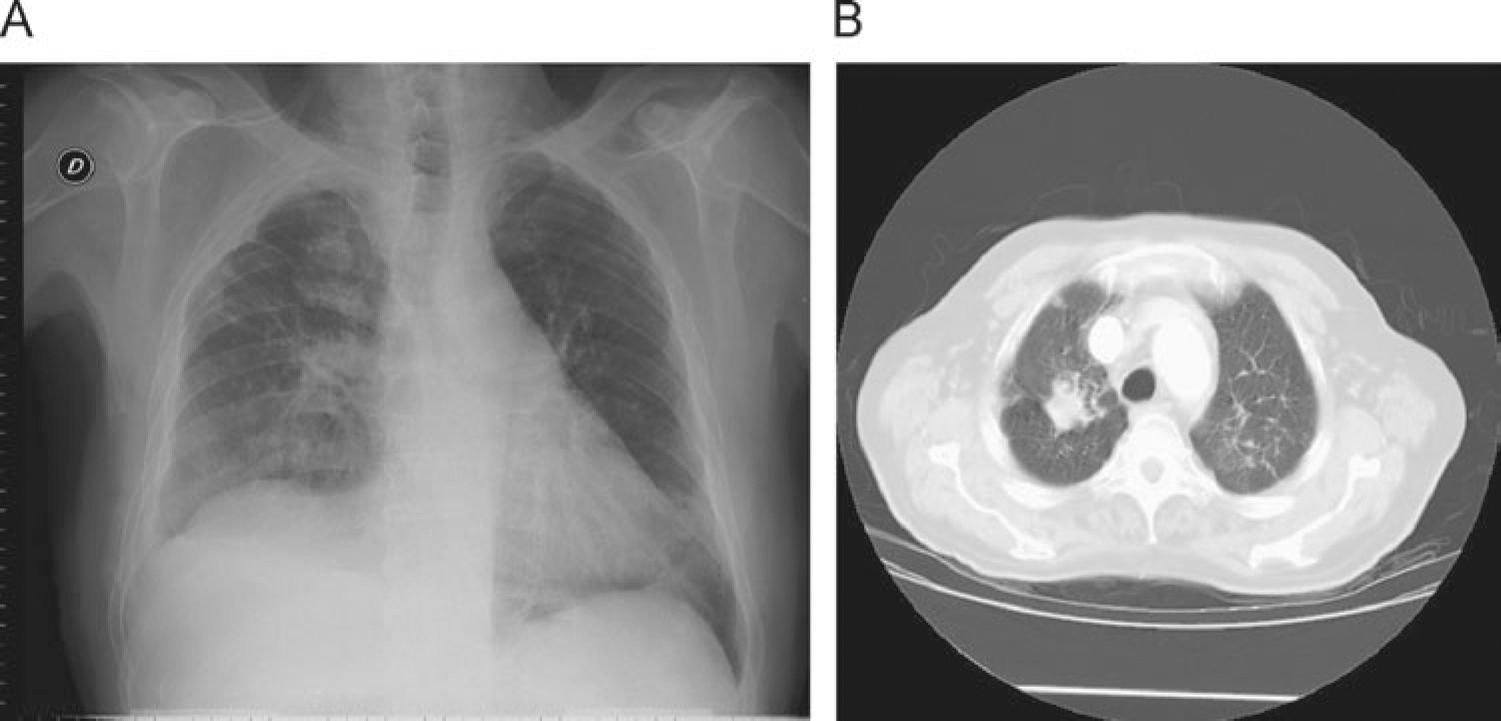
We present the case of a 79 year old man with a history of prostate a history of prostate cancer, arterial hypertension, chronic lymphatic leukaemia and atrial fibrillation. He is an ex-smoker (1 pack-year smoking history 20 years ago) and worked in a brewery for 27 years, having retired 9 years ago. He has been admitted with a respiratory infection and coughed up blood. On admittance BP: 160/70 mmHg. Heart auscultation detected arrhythmia of 120 beats per minute, respiratory auscultation found a general decrease of normal breathing sounds which were slight without any added noises. In additional tests requested it was noted that leukocytosis was 16,100/ul (neutrophils: 38%, lymphocytes: 50%), and there were no significant alterations of coagulation and biochemical values. A chest X-ray (fig. 1A) showed: Enlarged heart with signs of vascular reconversion, fibrous tracts of a residual aspect in the right upper lobe (RUL) and right para-tracheal node and a chest CT (fig. 1B) showed signs of pre-capillary hypertension, fibrous tracts in the apical region of the RUL. These findings had already been detected in previous studies 2 years before and had not worsened according to X-ray images. The Image was compatible with a 24×27 mm node in the RUL that contained a small cavitated image. Some mediastinal adenopathies of up to 15 mm in diameter were found in the precarinal region. The patient underwent a Mantoux test and bacterial testing (3 samples) that were negative. Clinical evolution was favourable with analgesic and antibiotic treatment, but given the smoking history, bloody cough and X-ray findings, a fibrobronchoscopy was performed. The most significant findings were vascular lacunae at the entry of the main right bronchus and some scar bands in the segmental bronchi of the URL bronchus. Respiratory function was normal on exploration. A PET scan was also performed which showed that a 29×35 mm node had formed in the URL with metabolism increase (SUV max 10.6) and changes in density, fibrous tracts and an increase in glycidic activity in the left upper and lower lobes, upper URL segment and middle lobe (SUV max 3.8,3.8,5.3, and 4.2, respectively). It was recommended that the histology of the node in the RUL be studied. A CT guided biopsy of the lung node was performed and the anatomopathological report stated that it was a proliferation compatible with lung silicoanthracosis.
Diatomaceous earth is an amorphous form of silica. It is formed by the skeletons of diatoms,2 which are microalgae that are covered with silica. When they die, their organic material degrades and their silica skeleton is deposited on the sea-bed. Once it is extracted and calcined this diatomaceous earth has several uses, among them, it is used as a filtering substance in the manufacture of beer, juices and wine. The relationship between the risk of silicosis and workers in industries that use diatomaceous earth has been described and established. This industrial exposure can take place both during its production and during the use of the substance.2–4 Most studies concentrate on patients who work with the extraction and calcination of this material. In a Pubmed search we did not find a description of any case of silicosis due to exposure to diatomaceous earth used for filtration in the beer manufacturing process. We obtained a very detailed anamnesis of work or domestic exposure from this patient and did not find any other exposure that he recognised as such. During the anatomopathological study, we also found indications of carbon exposure. However, the patient denied any type of exposure to this mineral either at work or at home.
With reference to X-ray alterations, it is important to point out that when silicosis is caused by diatomaceous earth it is possible to see a reticular pattern which is not frequently seen in other circumstances.5
PET scans are not useful for differential diagnosis of lung neoplasms since it has been possible to see a high uptake of progressive massive fibrous masses and silica adenopathies,6 and, in fact, they are a source of false positives.
To summarise, the sources of exposure to silica are numerous, they are present in many industries and some of them are not recognised (as in this case). A detailed anamnesis of patients' work history is required since there are unusual sources of silica exposure that can, nevertheless, cause disease.