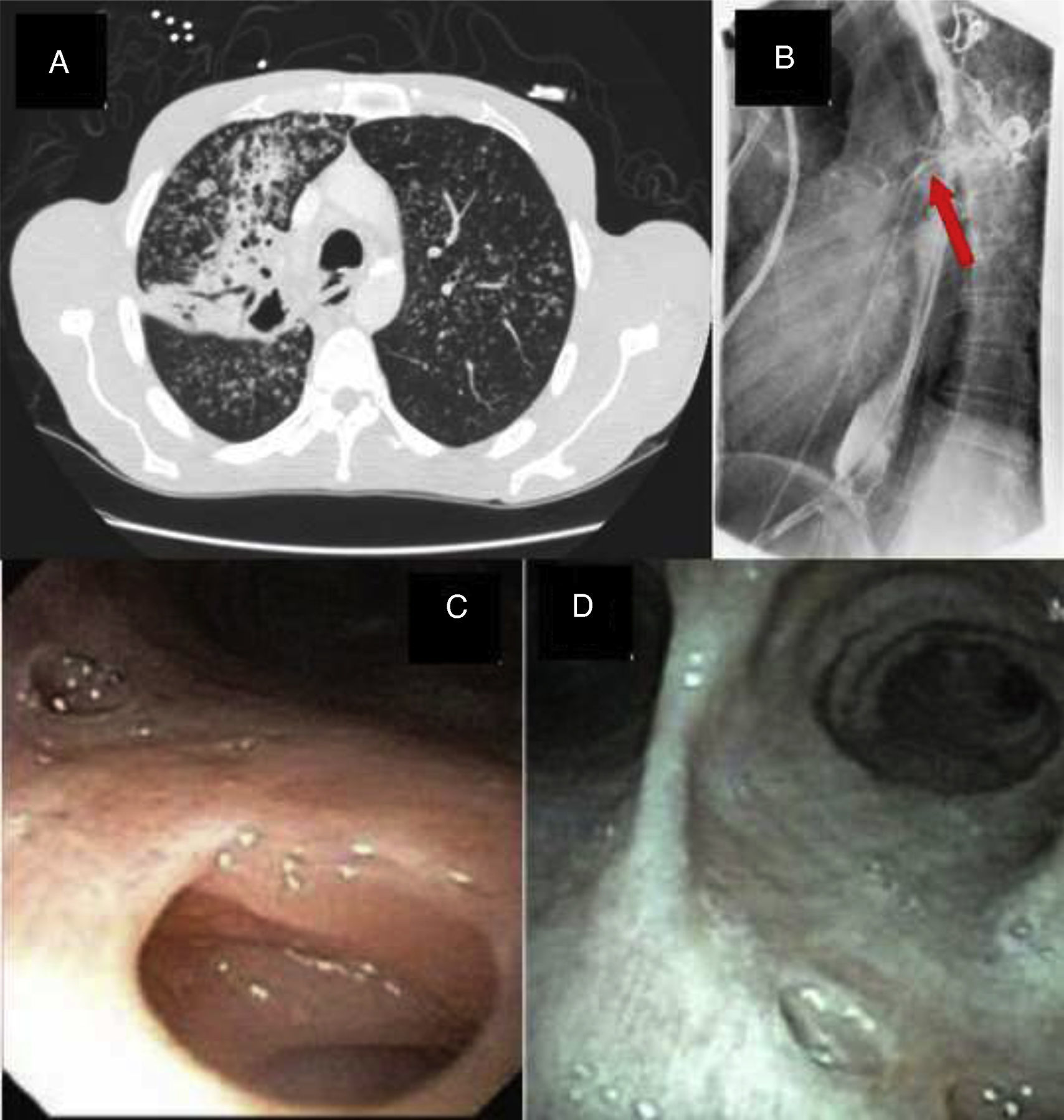
A 46-year-old male, HIV seronegative, smoker, with non-insulin dependent diabetes mellitus presented with complaints of cough, weight loss and dysphagia of six months’ duration. Chest X-ray, followed by CT scans (Fig. 1A) revealed a right upper lobe cavity with a fistulous communication between the trachea and esophagus. Sputum stains were positive for acid fast bacilli consistent with Mycobacterium tuberculosis and the patient was started on antituberculous treatment. A barium esophagogram revealed the presence of a fistulous tract from the esophagus (Fig. 1B), following which an endoscopic gastroduodenoscopy showed a 2.5cm defect in the upper esophagus with a visible fistulous track. Bronchoscopy demonstrated the fistulous tract at the distal right posterior trachea (Fig. 1C). He was managed conservatively with percutaneous gastrostomy feeding and discharged on direct observed therapy for tuberculosis with Rifampicin, isoniazid, pyrazinamide, ethambutol and vitamin B6. After 6 months of treatment, his dysphagia resolved. A repeat barium esophagogram and bronchoscopy (Fig. 1D) showed interval healing of the tracheoesophageal fistula.
Tracheoesophageal fistulas mostly occur as an acquired complication due to malignancy, granulomatous infections, trauma and post endotracheal intubation. Tracheoesophageal fistulas caused by tuberculosis are an exceedingly rare complication, and have been postulated to occur secondary to rupture of caseous peribronchial lymph nodes into adjacent mediastinal structures with subsequent fistula formation. The best course of management is unclear. While certain cases have been managed surgically,1 others reported successful resolution of the fistula with medical management alone2 as seen in our case.