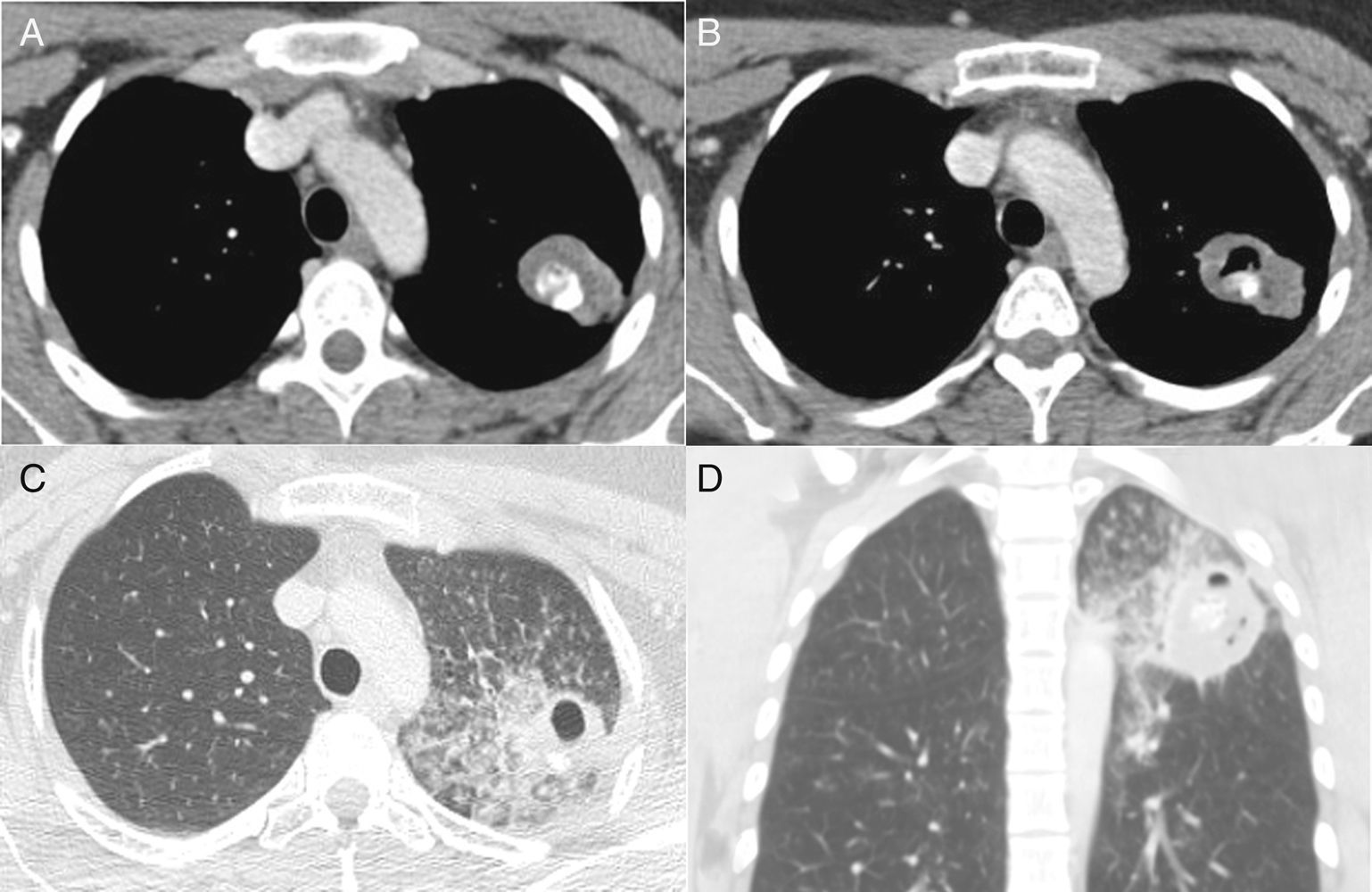
A 28-year-old non-smoking woman presented with an abnormal chest radiograph acquired during a routine check-up. The patient had a history of pulmonary tuberculosis treated 20 years previously. Computed tomography (CT) of the thorax revealed a nodular lesion containing a focal calcification, located in the apicoposterior segment of the left upper lobe (Fig. 1A). The diagnosis of granuloma due to tuberculosis was suggested. The patient refused surgical treatment. The lesion was followed clinically. Eight months after the initial CT examination, the patient was admitted with productive cough, weight loss, and low-grade evening fever. A new CT examination showed cavitation of the previously observed nodule, with adjacent opacities, suggestive of reactivation of the infectious process with bronchial dissemination (Fig. 1B–D). The patient's sputum was positive for acid-fast bacilli and a culture was positive for Mycobacterium tuberculosis.
Chest CT image obtained with the mediastinal window setting (A) shows a nodular soft-tissue lesion with internal calcification located in the apicoposterior segment of the left upper lobe (tuberculoma). CT images obtained with the lung window setting (B–D) 8 months later show cavitation of the nodule associated with focal consolidation, ground-glass opacities, and airspace nodules, indicating reactivation and dissemination of the infection.
Tuberculoma is one of the most common benign pulmonary nodules. In general, these nodules are well defined, round or oval solitary lesions that frequently present with calcifications and/or small peripheral (satellite) nodules.1,2 There is no clear consensus on tuberculoma management strategy.
Although tuberculoma is a relatively common finding in patients with pulmonary tuberculosis, its cavitation and reactivation of the infectious process are rarely documented in imaging studies.