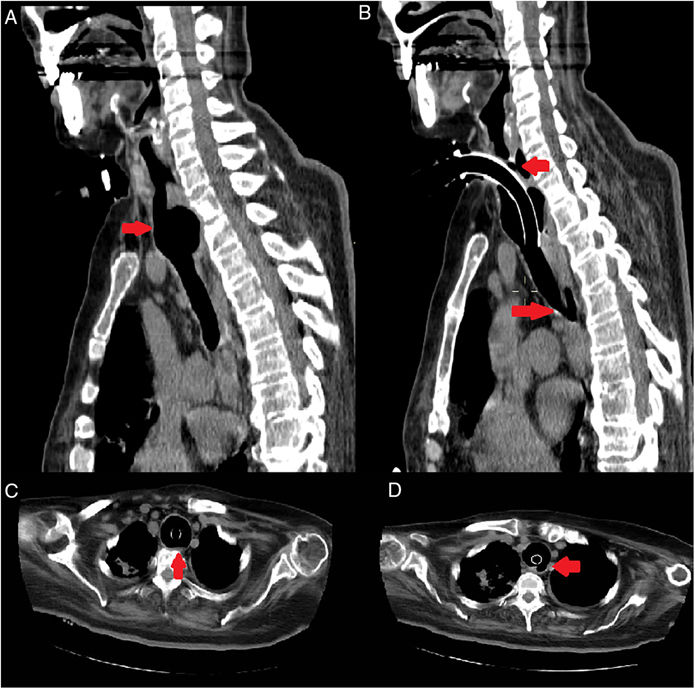
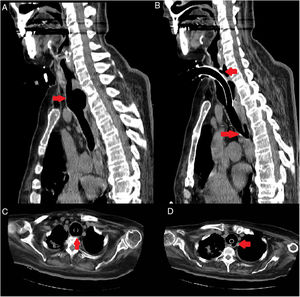
We report the case of a 67-year-old woman diagnosed with amyotrophic lateral sclerosis in 2008, who has needed enteral feeding by percutaneous endoscopic gastrostomy (PEG) since 2010 and invasive mechanical ventilation (MV) via tracheostomy since 2015. In 2018, after 3 years on MV, she attended the emergency room due to fever. Food content was found to be exiting through the tracheostomy. Chest computed tomography (CT) revealed a 5 × 2.6 mm tracheoesophageal fistula in the left posterolateral region of the trachea along with tracheal dilation at the cannula insertion site (Fig. 1). A tracheal cannula was implanted to bypass the path of the fistula, but given the patient’s poor clinical improvement and personal history, the decision was made to limit the therapeutic effort.
Tracheoesophageal fistula is an uncommon complication, occurring in between 0.3% and 3% of tracheostomized patients. It is caused by prolonged pressure exerted by the balloon of the tracheostomy cannula on the posterior wall of the trachea causing ischemia and necrosis of the area.1 It should be considered when abdominal bloating, bronchoaspiration, or coughing appears when swallowing.2 In our case, although the patient was fed by PEG, repeated bronchoaspiration could not be avoided.
Please cite this article as: Louvier RP, Bernáldez CB, Gómez JFS, Fístula traqueoesofágica secundaria a ventilación mecánica prolongada. Arch Bronconeumol. 2020;56:593.