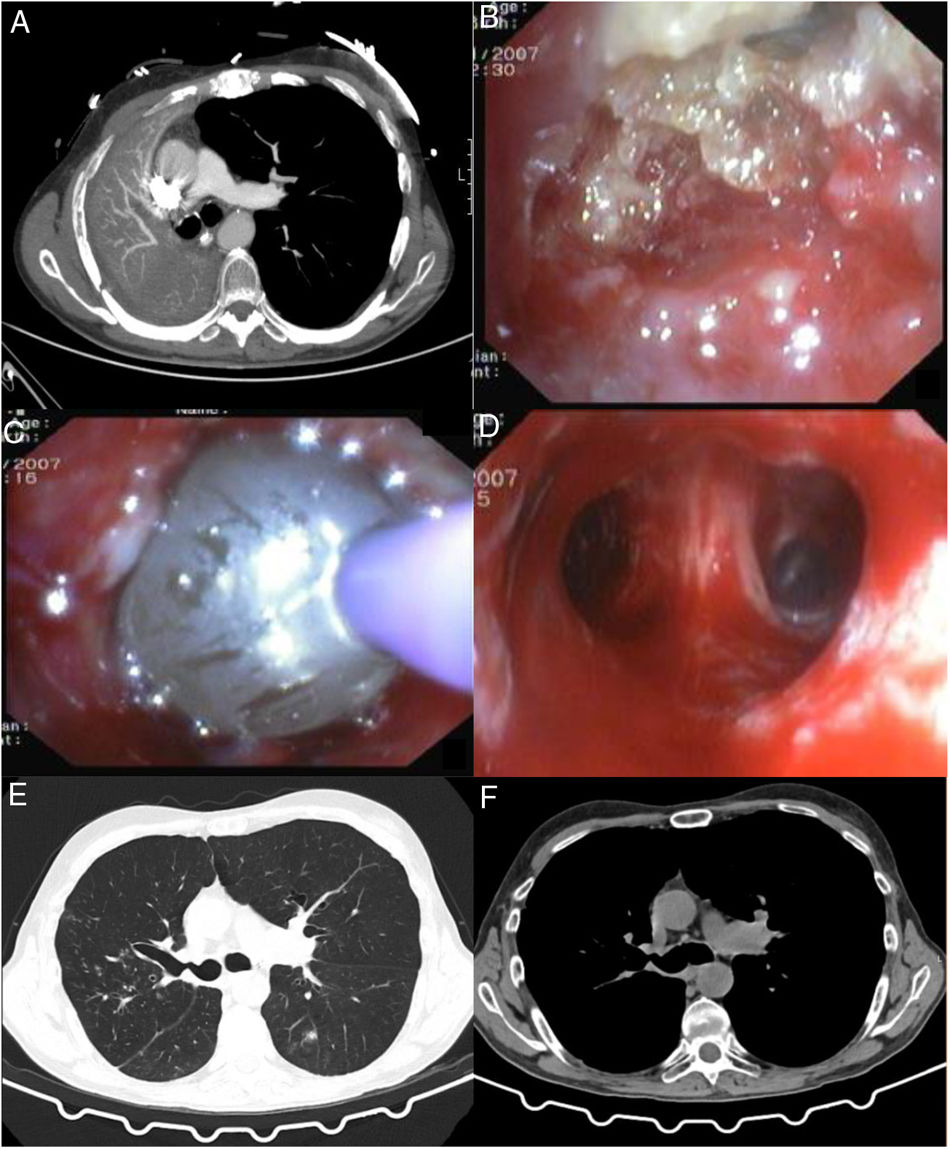
The authors report the case of a 54-year-old male patient submitted to bipulmonary transplant due to chronic obstructive pulmonary disease. According to surgical registries, a continuous running suture on membranous and an interrupted suture on cartilaginous portion of bronchus was made. Surveillance bronchoscopy was performed during the first three months without evidence of airway complications. The patient was immunosuppressed with tacrolimus and mycophenolate. Eight months after transplantation, he developed dyspnea, and functional tests showed marked FEV1 decreased. Chest CT detected complete atelectasis of right lung (Fig. 1A) and bronchoscopy occlusion of right main bronchus by a yellowish hard mass (Fig. 1B). Histological and microbiological examination confirmed Aspergillus infection. The patient underwent rigid bronchoscopy with mechanical desobstruction (Fig. 1C and D) and began therapy with amphotericin B followed by posaconazole. A follow-up CT image, four months after, showed marked improvement with resolution of atelectasis, however, with a stenosis in the emergence of right upper lobar bronchus (Fig. 1E). The patient maintains endoscopic and microbiologic surveillance, according to clinical and functional evolution.
Aspergillus infections are common following lung transplantation, with diverse and complex manifestations.1,2 Anastomotic infections should be a complication to fear despite antifungal prophylaxis. Routine bronchoscopy plays an important role, not only as a means to diagnose but also for therapeutic purposes, namely in early diagnosis of suture complications.