IgG4-related disease is characterized by lymphoplasmacytic infiltration of IgG4+ plasma cells due to Th2 cell-B cell interaction. In 60%–80% of patients, it is associated with elevated serum IgG4 levels.1–3 It occurs more commonly in women, and clinical manifestations are multiple: tubulointerstitial nephritis, pancreatitis, cholangitis, liver disease, cervical fibrosis, orbital inflammation, middle-ear inflammation, sialadenitis, skin manifestations, mastitis, retroperitoneal fibrosis, prostatitis, lymphadenopathies, thyroiditis, hypophysitis, pachymeningitis, pericarditis, etc. The only respiratory manifestation that has been described is interstitial lung disease.1,4 We report 2 cases with previously unreported pulmonary involvement in the form of tracheal stenosis.
A 60-year-old woman with chronic interstitial nephritis had been receiving immunosuppressants until 6 months previously. She had also been diagnosed with asthma 7 years previously, and consulted due to poor asthma control since discontinuing her immunosuppressive treatment. Stridor and moderate obstructive ventilatory changes characterized by an upper airway obstructive pattern were observed. Chest computed tomography (CT) was normal, but bronchoscopy revealed circumferential stenosis in the lower margin of the cricoid and the first tracheal ring, measuring less than 1cm in length and smallest diameter estimated at 6.8mm. The tracheal stenosis was surgically resected, and the pathology report of the specimen revealed angiocentric fibrosis and subepithelial obliterating vasculitis of the trachea consistent with IgG4-related disease. IgG4 levels were normal, but the IgG4/IgG ratio was high.
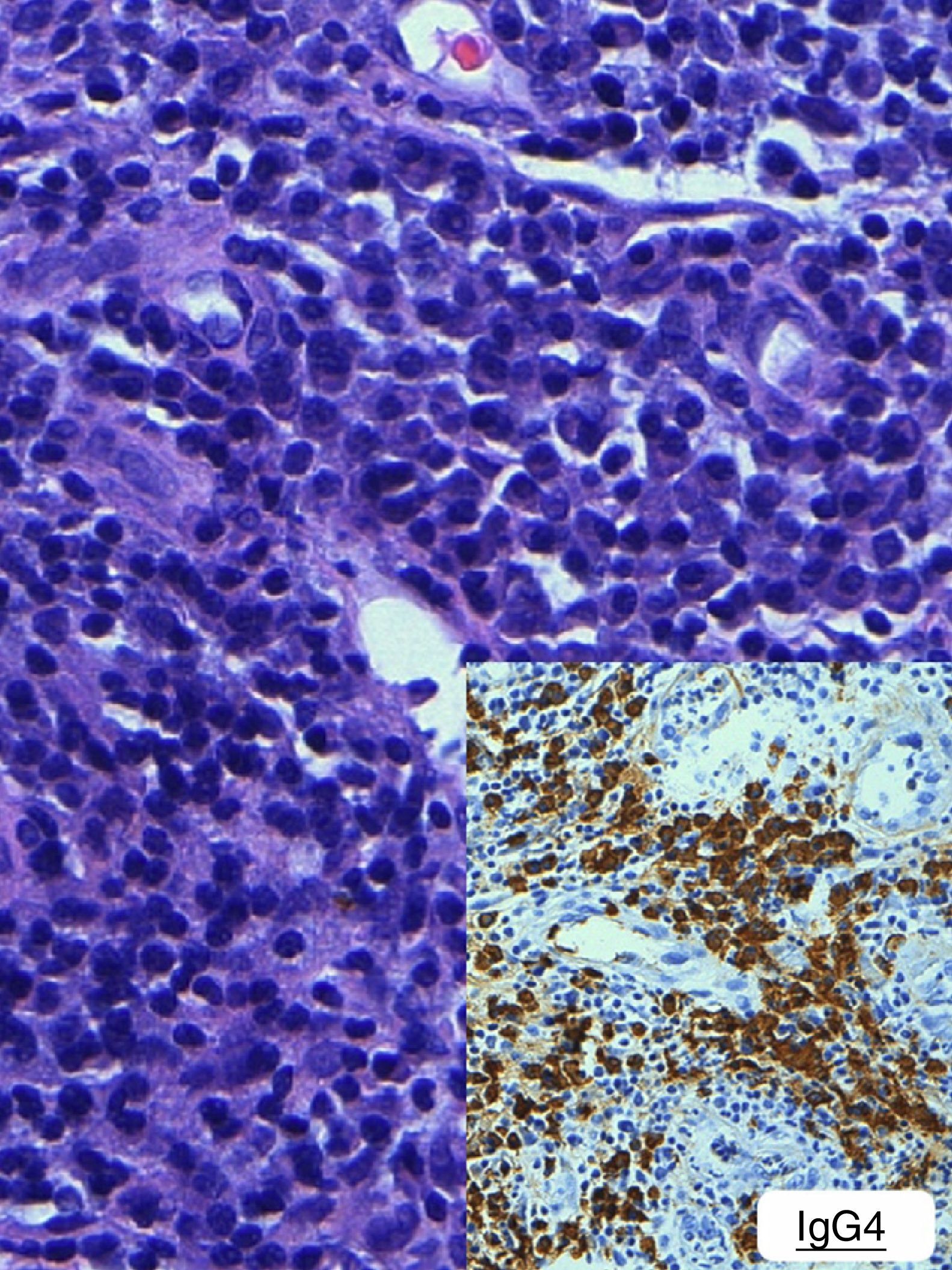
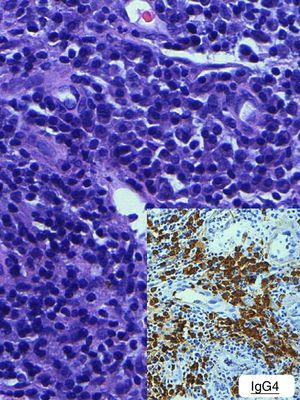
Our second case concerns an 85-year-old woman, with a 2-year history of dyspnea and recent onset of stridor. A cervicothoracic CT found concentric thickening of the trachea in the first ring, reducing the tracheal lumen by 50%. These findings were confirmed on bronchoscopy, during which biopsies of the stenosis were obtained. Results showed intense lymphoplasmacytic infiltration and subepithelial angiocentric fibrosis of the trachea, suggestive of IgG4-related disease. The patient's immunohistochemical profile was also consistent with IgG4 disease (>100 plasma cells with intense expression of IgG4/high-powered field (HPF) – the established diagnostic limit is 10/GCA) (Fig. 1).
Diagnosis is based on the histopathology of the affected tissue, showing lymphocyte and plasmocyte IgG4+ infiltrates greater than 10/HPF or IgG4/IgG+>40%, with no neutrophil infiltrate, and storiform (whorled) fibrosis and/or obliterative phlebitis.1–3 Up to 30% of patients can have normal IgG4 serum concentrations, even if histopathology criteria are met. Monitoring of IgG4 serum concentrations during the course of the disease may be useful for diagnosing relapses.1
Treatment with glucocorticosteroids relieves symptoms, reduces lesions, improves the function of affected organs, and reduces IgG4 serum concentrations. Azathioprine, mycophenolate and rituximab have also been used in refractory cases.1,4 Both our patients were treated with corticosteroids, and they are both currently asymptomatic.
This is a new manifestation of IgG4-related disease, which we feel should be included in the differential diagnosis of tracheal stenosis.
Please cite this article as: Comeche Casanova L, Ortega de Vitoria L, Moradiellos J. Estenosis traqueal y enfermedad por IgG4. Arch Bronconeumol. 2016;52:175.