Tracheal injury is a common complication after long-term tracheostomy, especially tracheal stenosis and tracheomalacia.1,2 Tracheal cartilage rings denudation is rare and there is a lack of cases reported in literature. The mechanism of tracheal injury is not well known, but it is thought to be caused by mechanical aggression of the tube and inflatable cuff, associated to a foreign body reaction on tracheal mucosa.3 The tracheal injury can be increased with the duration of tracheostomy, cuff properties/inflation pressure and infection of tracheal stoma.4 Animal models suggest a histopathological association with different types of tracheal injury.3,4 In this sense, Nottingham Compositive Tracheal Injury Scoring propose a histopathological scoring system which provides quantifications of injury in the various layers of tracheal tissue.4
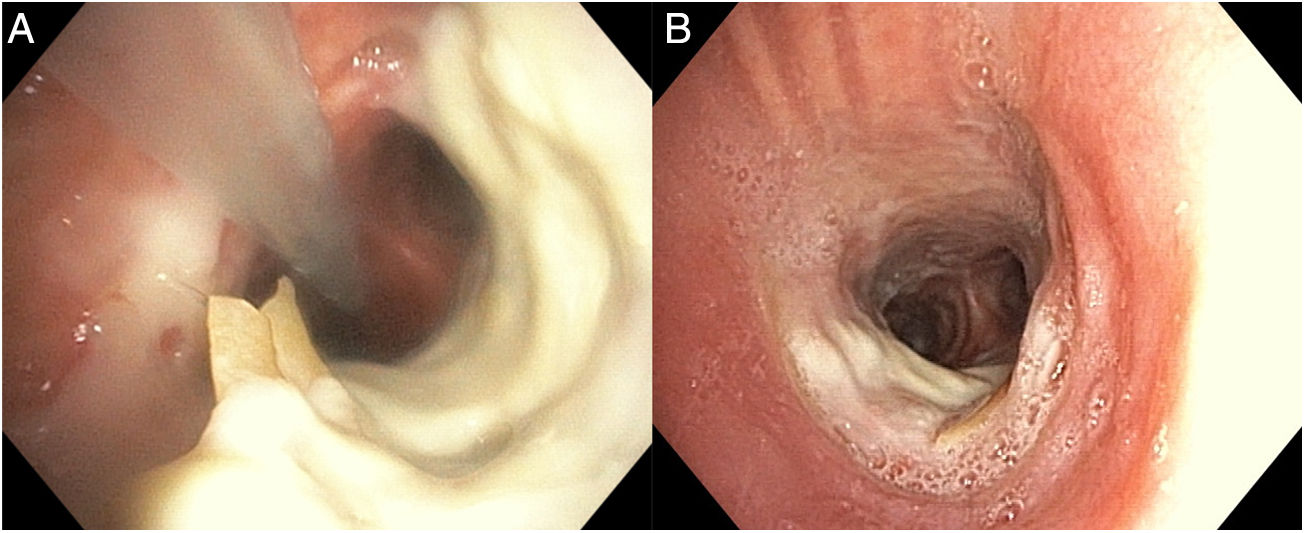
A 63-year-old woman, non-smoker, with a past medical history of type 2 diabetes mellitus was admitted to intensive care unit with cardiogenic shock due to acute decompensated heart failure. The patient was on ventilatory support for 44 days. On day 12, due to prolonged orotracheal intubation, a bedside percutaneous dilatational tracheostomy (guide wire dilating forceps technique) guided by flexible bronchoscopy was performed. No immediate or maintenance related complications were noted. Cuff pressures were maintained on accepted range (20–30cmH2O). Following tracheostomy decannulation, a difficulty in closing tracheal stoma and abundant secretion release were reported. Flexible bronchoscopy was performed and revealed necrosis of the anterior wall of the mid-trachea, associated with an exposure of two cartilage rings with right edges detached from the wall (Fig. 1A). Histological assessment of a small fragment of cartilage showed hyaline cicatrization. The patient started systemic corticotherapy (prednisolone 1mg/kg/day). Flexible bronchoscopy was repeated 3 weeks later and showed a reduction of necrosis areas and re-epithelialization of inner surface of denudated cartilage rings, without evidence of stenosis (Fig. 1B). The hospitalization was prolonged due to a nosocomial pneumonia. After an 89-day hospital stay, the patient was transferred to a rehabilitation unit with bronchoscopy follow-up scheduled after 2 months. Unfortunately, she died 1 month later due to acute pulmonary embolism.
Due to the unusual cases of tracheal ring denudation, its evolution is poorly known. And while we were able to observe a re-epithelialization of cartilage ring without tracheal stenosis a month after decannulation, it was not possible to assess a long-term evaluation. This goes accordingly with what is postulated by Welkoborky et al. that superficial injuries affecting inner tissue layers have a great capacity to regenerate and that the depth of the airway damage is more critical than the extent or length to the development of tracheal stenosis.2 Although histopathological finds are difficult to assess, they appear to be crucial to understand the development of different complications.
FundingNo funders pertaining to this article.