In childhood, pneumonic processes are frequent and the existence of pleural complications is not uncommon, but the appearance of lung abscess is rare and potentially severe. Nevertheless, most respond well to conservative treatment with antibiotics, and surgical management is reserved for those cases in which it antibiotics are not sufficient.1,2 Lung abscess surgery, mainly segmentectomy or open lobectomy, presents high morbidity and mortality. This has led to the appearance of other alternatives, such as percutaneous or endoscopic drainage of the abscess.1–5 In our department, we have opted for thoracoscopy. We present 2 cases that have occurred in 2005 and 2008.
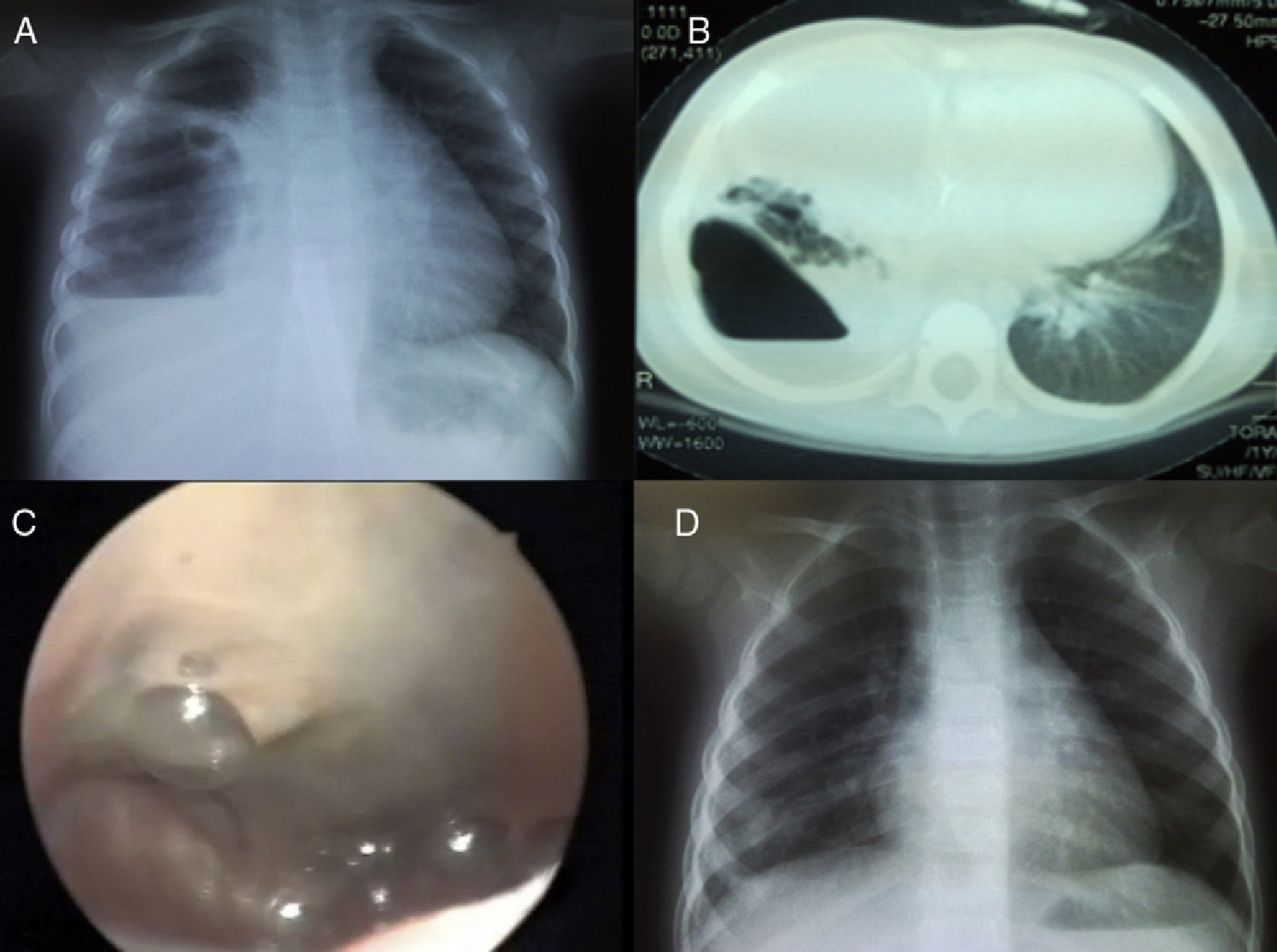
Case 1: A 23-month-old girl was admitted to our hospital due to 4 days of fever and diagnosis of pneumonia in the right lower lobe (RLL). She had been treated in the ambulatory setting with azithromycin, but showed no improvement. After 8 days of hospitalization and treatment with intravenous cefotaxime, radiology revealed the appearance of bullous images and air fluid level. CT was ordered, which showed large destructive parenchymal lesions in the RLL compatible with lung abscess, empyema and the existence of air in the pleural cavity due to a possible bronchopleural fistula (BPF). We decided to use a surgical approach with thoracoscopy and two 5-mm ports of entry under general anesthesia with conventional intubation and insufflation of CO2 at a pressure of 6mmHg. The findings were intense fibrinous adherences and a necrotic area in the RLL with a BPF measuring 2mm in diameter. We thus carried out debridement of the empyema, incision of the abscess, aspiration of the purulent material and intracavitary lavage with saline solution, leaving the drain in the pleural space.
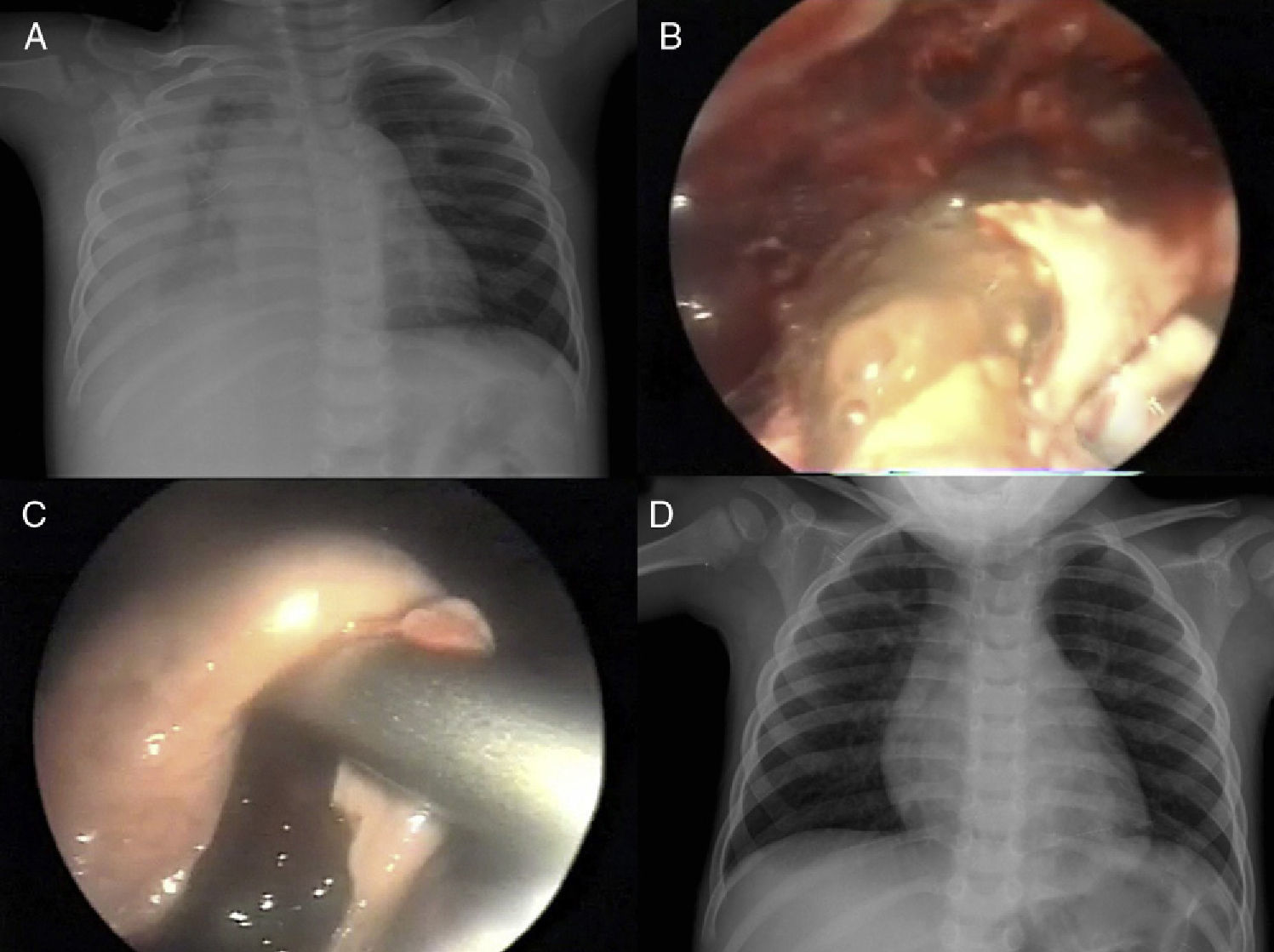
Case 2: A 22-month-old boy was hospitalized for fever and cough that had been evolving over the previous 3 days, which was diagnosed as pneumonia of the right upper lobe (RUL) that was complicated by pleural empyema. Systemic antibiotic treatment was begun with cefotaxime and vancomycin, along with pleural drainage and fibrinolytic therapy. As there was no improvement in the symptoms, thoracoscopy was performed on the eighth day of hospitalization, with a finding of lung abscess in the RUL that was debrided and drained. In this case, selective intubation was not done, and the entry of the previous pleural tube was taken advantage of in order to insert another port, meaning 3 were used.
After surgical intervention, clinical and radiological improvements were seen in both patients, and fever disappeared on the third and fourth post-op days, respectively. Post-operative intravenous antibiotic treatment was maintained for 2 weeks in the two cases and the pleural drain was withdrawn a week after the surgical intervention in the first case, with resolution of the BPF, and after 12 days in the second case. As the only complication, the second child presented pneumothorax in the early post-operative period due to obstruction of the pleural drain, which was resolved without incident. The hospital stays were 24 and 27 days, respectively. After the patients had been discharged, immunity studies were done to rule out immune deficiency (Figs. 1 and 2).
(A) Chest radiography demonstrating a cavity with air–fluid level in its interior in the right hemithorax. (B) Pre-operative CT shows a lesion compatible with abscessed necrotizing pneumonia in the right lower lobe. (C) Intraoperative image of the lung abscess; note the greenish appearance of the parenchyma and the surrounding air bubbles caused by the BPF. (D) Radiological check-up 2 months after surgery.
(A) Pre-operative thoracic radiography with right empyema reaching the lung apex. (B) Thoracoscopic image showing the drainage of the content of the abscess. (C) Intraoperative image of the cavity of the abscess after the evacuation of the detritus. (D) Radiological check-up 2 months after surgery.
Traditionally, surgical treatment of lung abscesses has presented high morbidity. Thoracoscopy may be a good alternative as it presents some advantages over the other techniques in peripheral abscesses that accompany empyema, because when the pleural cavity is accessed the empyema can also be resolved. It is able to safely access peripheral lesions, make the incision and directly drain the cavity of the abscess, without needing to unroof it. It is true that it is necessary to subject children to general anesthesia, but it is also usually necessary in order to safely perform percutaneous or endoscopic aspiration of abscesses.1,3
Please cite this article as: Garrido-Pérez JI, et al. Utilidad de la toracoscopia en el tratamiento del absceso pulmonar en la infancia. Arch Bronconeumol. 2012;48:382–3.