Splenosis is a benign condition characterized by ectopic splenic tissue following traumatic rupture of the spleen or splenectomy.1 Thoracic splenosis is rare and almost exclusively present in the left hemithorax. Patients are usually asymptomatic, and it is most commonly an incidental finding.2 Diagnosis is challenging as the multiple nodules could mimic malignancy and because there is a long interval between initial trauma and diagnosis.1 Management is expectant except in symptomatic patients or whenever the diagnosis of splenosis is unclear.2
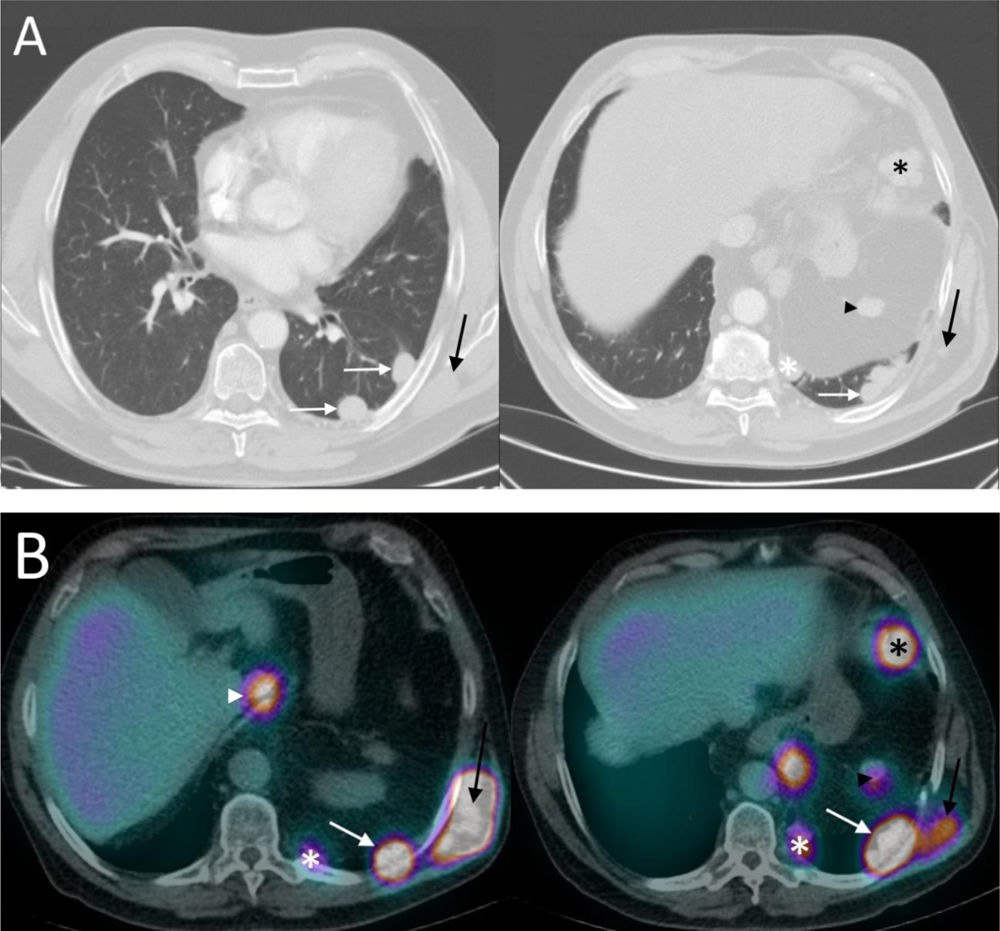
A 66-year-old male with a history of splenectomy after a car accident presented 40 years later with asymptomatic opacities in the left hemithorax on routine chest radiography. Chest computed tomography (CT) showed scattered nodules in the left pleura, in the mediastinum, in the left posterior chest wall, medial to the liver, at the previous splenic site and in the left diaphragm (Fig. 1A). SPECT/CT with technetium (Tc)-99m showed increased uptake by the same nodular formations (Fig. 1B). History and the preferential distribution of the nodules in the left hemithorax and the presence of splenic orthotopic spleen tissue were sufficient to establish the diagnosis of thoracic and abdominal splenosis. Given the asymptomatic state, conservative treatment and follow-up was performed.