A 56-year-old hypertensive gentleman with a 40 pack-year history of smoking was diagnosed with chronic obstructive pulmonary disease (COPD) characterized by GOLD-E and Grade 4 obstruction. Despite pulmonary rehabilitation and optimized inhaler therapy (glycopyrronium/indacaterol/beclomethasone), he remained symptomatic and primarily wheelchair-bound with modified medical research council (mMRC) scale of three and he could only walk for 80 meters on six-minute walking test (6MWT). He had three non-infective exacerbations requiring admission in the last twelve months. His forced expiratory volume in the first second (FEV1) was 0.82l (26% predicted) and forced vital capacity was 2.78l (70% predicted), with an FEV1/FVC ratio of 0.29. Plethysmography indicated severe air trapping [residual volume (RV) 192% predicted, total lung capacity (TLC) 100% predicted, RV/TLC ratio 0.55], and diffusing capacity for carbon monoxide (DLCO) of 43% predicted. Transthoracic echocardiography showed no pulmonary hypertension. Arterial blood gas analysis revealed hypoxemia (pO2 72mmHg) without hypercapnia (pCO2 32mmHg).
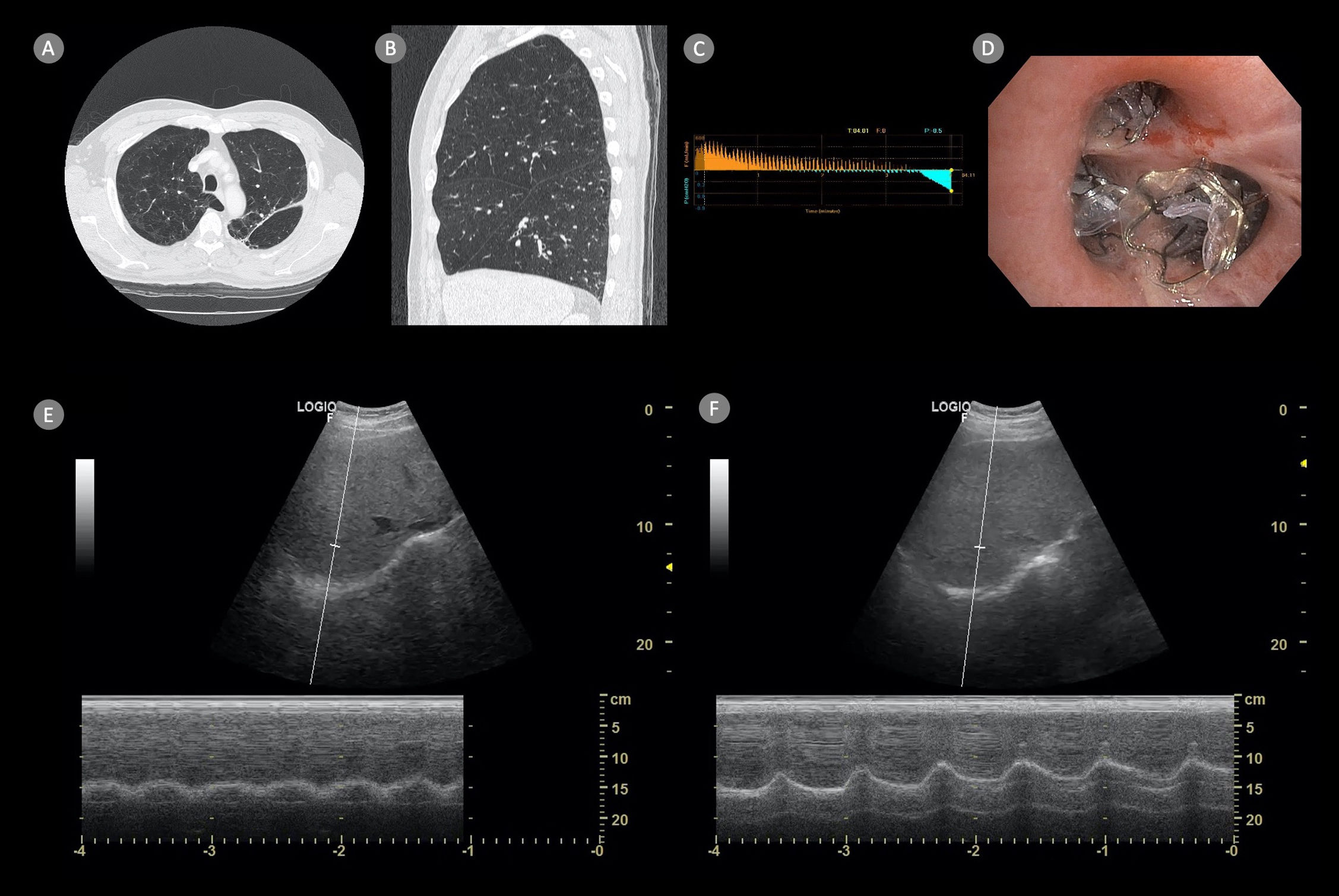
Quantitative CT (QCT) thorax confirmed upper lobe-predominant, heterogeneous emphysema with an intact fissure (98% completeness over right oblique fissure and 100% completeness over right horizontal fissure) over the right lung (Fig. 1, Panel A & B). Pre-procedure, right-hemi diaphragmatic excursion measured 3.35cm with a sniff maneuver in 45° semi-recumbent position (Fig. 1, Panel E). Under total intravenous anesthesia, three endobronchial valves were placed in the segmental bronchi of the right upper lobe after confirming no collateral ventilation (Fig. 1, Panels C & D). Post-procedure, pneumothorax occurred within 24h, necessitating an intercostal chest drain for 10 days. Patient was discharged uneventfully.
High-resolution CT thorax showing upper lobe predominant heterogeneous emphysema with centrilobular distribution in the right lung (Panel A) and complete fissure integrity (Panel B). Absence of collateral ventilation confirmed by occlusion of the right upper lobe ostium with the Chartis® balloon (Panel C). Deployment of three endobronchial valves in the anterior, posterior, and apical segments of the right upper lobe (Panel D).
Two weeks post-procedure, right hemi-diaphragmatic excursion increased to 4.50cm (+34%) (Fig. 1, Panel F; Video 1). A follow-up chest radiograph at one month showed complete collapse of the right upper lobe, accompanied by improvements in FVC (+1.05l), FEV1 (+0.50l), RV (−2.12l), and a significant increase in 6MWT distance (+280m). Clinically, the patient's mMRC scale improved to one, and he could engage in moderate physical activity.
Lung hyperinflation in severe COPD often leads to impaired respiratory muscle function, particularly the diaphragm, which will translate to significant functional limitation as diaphragm is the most important primary respiratory muscle.1 Bronchoscopic lung volume reduction (BLVR) using endobronchial valves is a minimally invasive procedure which is non inferior to lung volume reduction surgery.2 While BLVR's impact on quality of life, lung function, and exercise capacity has been extensively studied, its effect on diaphragmatic motility remains less explored. However, assessment of diaphragm function via ultrasound can be operator-dependent with high variability, our case suggests that BLVR can potentially improve diaphragm mechanics. Therefore, further research to evaluate the utility of bedside ultrasound in assessing BLVR outcomes during both short and long-term follow-ups, especially its effect on diaphragmatic function, may be warranted.
FundingThe authors declare that no funding was received for the publication of this case.
Authors’ contributionSSK initiated the idea for manuscript submission and prepared the final copy of the manuscript. SSK, SKI acquired the clinical data. SSK performed the transthoracic ultrasound. SSK, SKI, STT were involved in the care of the patient. All authors have read and approved the final manuscript.
Conflicts of interestThe authors have no conflicts of interests to declare.