Obstructive sleep apnea (OSA) is the most prevalent respiratory disorder during sleep, affecting more than 20% of the adult population.1 It is a chronic and frequent disorder, with manifestations of excessive daytime sleepiness, fatigue, and poor quality of life. For the treatment of symptoms associated with OSA, continuous positive airway pressure (CPAP) has been shown to be a clearly effective and cost-effective therapy. OSA has also been linked to an increased risk of cardiovascular disease, cerebrovascular disease, and high blood pressure (BP).2 Considering such risks, the benefit of CPAP treatment is not evident in all conditions, however several observational studies have found an increased incidence of hypertension and cardiovascular disease in patients with OSA, while intervention studies on CPAP have shown disparate results in terms of the effect of OSA treatment.3
The heterogeneous effect of CPAP on cardiovascular morbidity in patients with OSA is multifactorial. On the one hand, CPAP is related to a decrease in BP, however in terms of secondary cardiovascular prevention, researchers have unanimously reported a neutral effect on reducing the risk of recurrent cardiovascular events.4 On the other hand, the heterogeneous effect observed in the intervention studies is also due to the incorrect classification of some patients due to the variability of the measure. This would be the case for the 24-h BP measurement, in which a variability of up to 30% has been reported between consecutive measurements on different days in the same patient.5 Moreover, apnoea–hypopnea index is used to assess the severity of OSA and because of its variability, researchers have found disparate results due to the measurement method or the performance on different days.6 This variability leads to incorrect classification of the patient and incorrect stratification of disease severity. Finally, it is necessary to consider the existence of different endotypes of the disease that may also explain the heterogeneity of the response.7,8 As in many other diseases, precision medicine has the fundamental challenge of characterizing these endotypes, with the aim of personalizing treatment.9,10 Deleterious effects have been reported in only certain patients with OSA. Therefore, it is necessary to identify patients with a certain endotype who would be vulnerable to the pathophysiological consequences of OSA to thus propose an intervention study that would demonstrate the beneficial effect of CPAP treatment.11
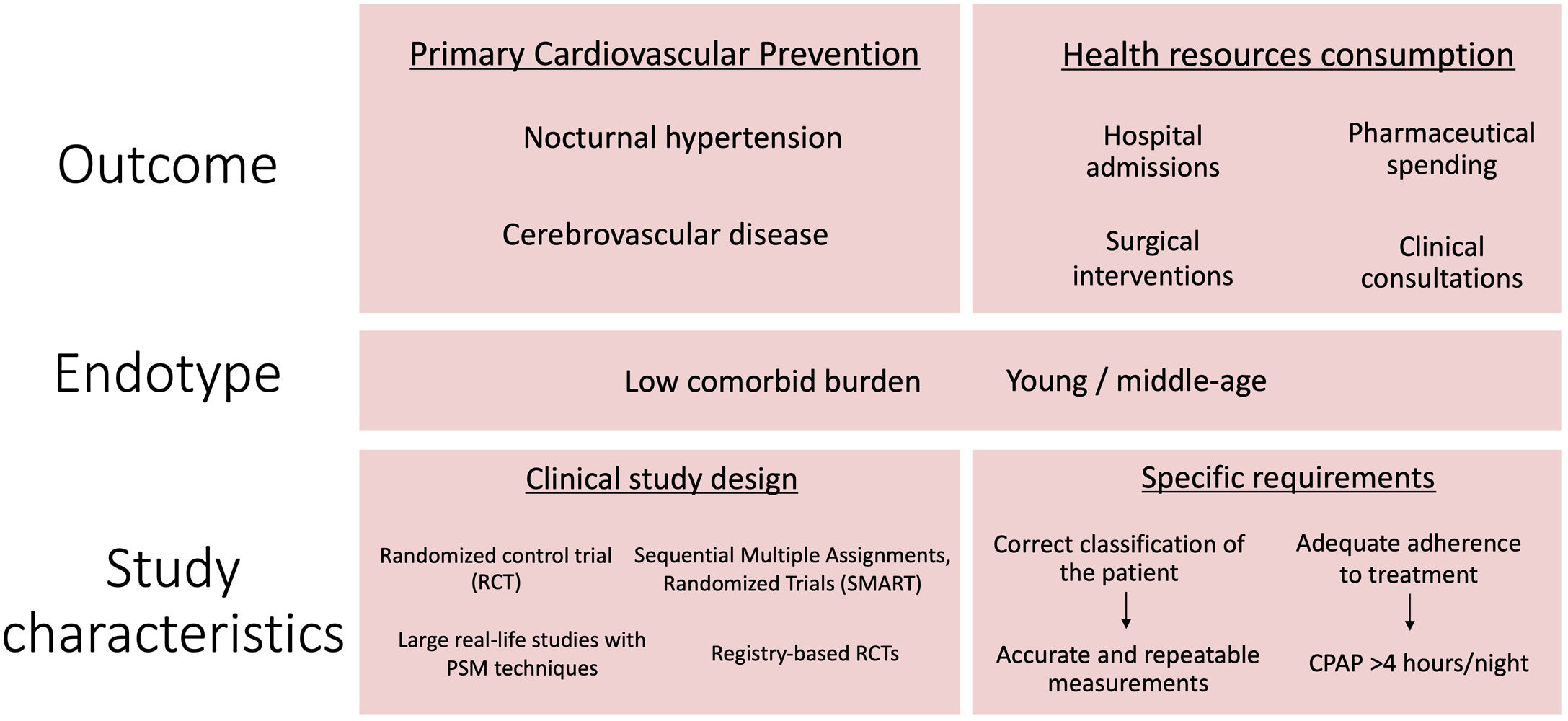
Considering the above, when proposing and designing new intervention studies, we must critique three fundamental aspects of the fundamental pillars of these new study designs. First, we must determine the measurement by which our clinical intervention will be assessed; second, we must clarify the classification and stratification of the patients and their disease, and perform precise and repeated measurements that allow us to strictly diagnose and classify each of the patients in our studies; and finally, it is essential that we describe the characteristics of the patient in whom we want to demonstrate the potential beneficial effect of our intervention because previous reports show that patients with said endotype are vulnerable to the deleterious effects of OSA.
The Spanish Sleep Network is a network in the field of OSA study, its effects, and the impact of its treatment.12 Currently, this cooperative network, like the rest of the international scientific community, faces the challenge of developing intervention studies that, based on the experience and evidence accumulated in recent years, allow us to specify and properly design our intervention with the objective to positively impact the health of our patients with OSA to reduce their cardiovascular risk. Among the members of the Spanish Sleep Network there is a broad consensus on the identification of primary cardiovascular prevention as one of the scenarios with a clear potential impact on the benefit of patients with OSA. Specifically, nocturnal hypertension is closely associated with OSA and has been proven to be an important and worthy topic of discussion.13 An intervention study showed that CPAP decreases on night-time BP in OSA patients with nocturnal hypertension, defined as a mean pressure greater than 120mmHg and/or 70mmHg during the hours of sleep. At this point, it is essential to consider the need for a correct diagnosis of patients with OSA and repeated 24-h BP measurements to correctly classify the study patients. Researchers have identified the potential of CPAP treatment in stroke prevention, and in previous studies, stroke prevention has been reported as one of the most ideal clinical outcomes of OSA treatment in patients with primary cardiovascular and cerebrovascular disease.14 Last, because patients with OSA have a chronic pathology, the clinical demand and consumption of healthcare resources are high.15 Thus, the decrease in the consumption of healthcare resources has been identified as one of the objectives to be considered in intervention studies on CPAP.
Another fundamental aspect to consider in the design of new intervention studies is the selection of study subjects with a low comorbid burden. In OSA patients without other cardiovascular comorbidities, cardiovascular pathology could be a modifiable independent risk factor, and treatment could have a significant impact if the main cardiovascular risk factor is eliminated. In addition, treatment adherence is another factor that has been unanimously considered fundamental to the success of CPAP intervention; the CPAP intervention is only expected to yield a positive effect in patients with a mean compliance time of 4–6h or more per night.16 The implementation of personalized programs aimed at adequate treatment adherence should be an important part of the methodological strategy of new intervention studies. Finally, it is necessary to consider new randomized study designs17 that, in addition to the inclusion of CPAP or placebo, consider other treatments sequentially for those patients who fail to adhere to these therapies. This is the goal of SMART (Sequential Multiple Assignments, Randomized Trials) study design.18 Additionally, considering the current economic burden of the intervention, we must consider other potential designs that rely on the examination of hospital clinical records. Clinical registries can be used to identify patients for recruitment, perform randomization, collect baseline variables, and detect targets of interest. Random assignment of patients in a clinical quality registry combines the features of a prospective randomized trial with a large-scale clinical registry. This is the case for registry-based randomized clinical trials.19 Moreover, it should be considered large observational real-life studies with propensity score matching statistical techniques to avoid the ethical problems that randomized clinical trials could suppose since very symptomatic patients cannot be randomized to placebo or no intervention for a long time (Fig. 1). The manipulation of these alternative designs could be useful in some of the proposed scenarios in terms of providing evidence of the therapeutic potential of OSA treatment.
The authors state that they have no conflict of interests.