With the acute first wave of the COVID-19 pandemic over,1 the long waiting list for sleep tests for OSA management has been further increased.2,3 The new preventive health measures against Covid-19 imply that patients go to the health centers as little as possible, which is why it is necessary to implement and start up a telematic workflow with home studies to guarantee sleep tests,4 especially CPAP titration.5–8 We aimed to test a new telematic workflow to deliver CPAP therapy to OSA patients and to evaluate it in terms of CPAP compliance, costs, residual events, symptoms and satisfaction of patients. The usual titration strategy has the following steps. The patient is scheduled to the daytime-hospital for information, and educational and practical training session with the device (45min). Then, our CPAP equipment is delivered to him/her for home titration (to be returned the next day), the data is downloaded, and a fixed pressure is prescribed. If the registration is incorrect, the titration is repeated another day. Finally, the patient is scheduled by the service company providing CPAP equipment that informs again how the equipment works, selects a final mask for treatment, and give a short practical session of the CPAP use.
The new telematic titration strategy was developed at 3 university hospitals—Clínic (Barcelona), Clínico Lozano Blesa (Zaragoza) and Bellvitge (L’Hospitalet del Llobregat) in collaboration with a healthcare provider company (Esteve-Teijin). By phone calls from the Sleep Unit, OSA-diagnosed patients waiting for CPAP titration were informed about the telematic process. Patients also received an email with detailed information and links to educational videos made by the group (sleep, hygiene, OSA and a real educational and training session similar as performed at the hospital) as well as written information of all the procedure. Subsequently, patients were addressed to the healthcare provider to pick-up their CPAP device (Dreamstation CPAP Pro, Respironics) with a suitable mask and to attend a CPAP educational as a practical session. CPAP devices were initially set to automatic CPAP mode (range: 6–12cmH2O) and equipped with a modem for remote data transmission and titration (EncoreAnywhere platform). The titration procedure was as follows. After the first night with CPAP treatment at home and for the following 2–3 days, a sleep technician telematically analyzed the automatic titration data from the A-trial program in order to set a fixed CPAP pressure value that normalized breathing (AHI<15 without major leaks). Patients received a phone call if massive leaks occurred based on the device data for>15% of sleep time or if CPAP use was<3h. If leak was moderate no action was performed. If central apneas appeared, CPAP pressure was fixed at 70% of the initial value suppressing obstructive events. If a final decision-making on CPAP pressure was not established until the end of the third day of therapy, it was considered as a re-titration. In addition, at the end of the first week all patients received a brief phone call from the nurse to identify and solve any possible complications with the treatment (nasal congestion and leaks among others). CPAP parameters could also be modified if needed. During the first month of treatment the sleep technician/nurse could call the patient to solve any possible problems. In addition, the patient could contact the Sleep Unit nurse at any time through email or voicemail to solve any problem. At the end of the first month with CPAP, the nurse performed a follow-up visit by phone or videoconference aimed to assess the main outcomes: CPAP compliance, residual events and symptoms such as snoring, restful sleep, witnessed apneas and Epworth sleepiness scale. The nurse could solve any possible problem. Patients also received a phone call from staff who was not involved in patient management to answer a satisfaction questionnaire (9 modified) about the titration procedure.
To analyze the usefulness of the telematic titration two procedures were considered: CPAP compliance and cost–effectiveness. Regarding compliance, two groups were analyzed. Compliance of the telematic titration group (n: 77) was compared with a historical cohort of 193 OSA patients from the year 2019 who were prospectively recruited from the 3 hospitals mentioned. Descriptive statistics were used for basic features of study data. Categorical variables were compared between groups (telematic vs control) using the chi-square test, whereas continuous variables were compared using the t-test or the nonparametric Mann–Whitney U test. Propensity score (PS)10,11 was used to obtain a 1:1 balance between patients in the telematic group (n=55) and control group (n=55). Linear regression analyses were also used to examine the associations between continuous clinical parameter AHI and telematic and control group. The Wilcoxon signed-rank test was used for comparing two continuous repeated measurements on the telematic sample (baseline vs 30-day), whereas categorical variables were compared using the McNemar test or the McNemar Bowker test.
The cost analysis of the procedure was performed only in patients of the Hospital Clinic (n:51) and compared with a recent hospital group in which cost was obtained with a similar group of study (n:38).9 Total direct (CPAP devices, material replacements, staff salaries, travel expenses) and indirect costs (patient's lost productivity) were evaluated considering changes in compliance analyzed in terms of costs and time spent by comparing the in-hospital routine vs telematic procedure using an objective Bayesian cost-effectiveness analysis where the effectiveness and the log tranformation of costs are assumed to follow a bivariate normal distribution.12
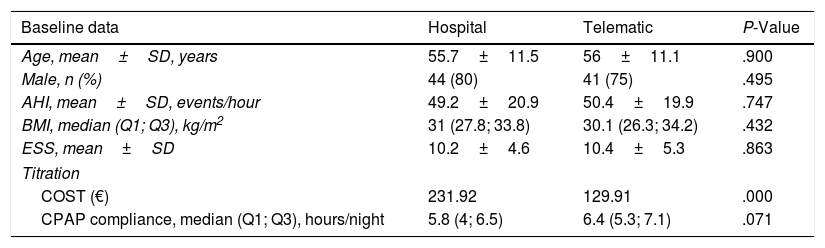
Main results were: 1. Compliance. In full cohort, telematic group patients (n=77) were younger with a lower BMI and ESS than in control group patients (n=193) (P=.035, P<.001 and P=.042, respectively). However, after PS matching, no significant differences were found in the baseline characteristics (Table 1). CPAP compliance showed similar values in the two groups in both full and PS matching cohort (P=.099 and P=.071, respectively); similar results were obtained using linear regression models, even after adjustment for center, in both full (P=.111 and padjusted=0.106) and PS matching cohort (P=.155 and padjusted=0.201). In telematic group, there were statistically significant differences between all baseline symptoms scores and 30-day symptoms scores (P<.001). 2. Cost: Telematic titration process was analyzed also in terms of costs and time spent by staff. To this end, we compared the in-hospital routine with the patients corresponding to the Hospital Clinic in Barcelona (n=51) showing that cost-effectiveness of remote titration was better, with similar compliance but lower cost (129.91€) than the hospital (231.92€). 58% of the costs of the telematic titration (75.65€ of 129.91€) are related to the first visit to the healthcare provider (CPAP device, educational session, travel expenses and loss of productivity by patients), and the 34% are related to the follow-up contacts and replacing masks and humidifiers. The costs of the first informative contact and the titration data analysis account for the 8% of the total costs. Bayesian cost-effectiveness analysis concluded that the telematic strategy was cheaper with a probability higher than 99.9% and more effective with a probability of 94.22%. Finally, the patients stated that they were satisfied with the new procedure, 95.8% were satisfied with the initial part of the treatment, 98.6% with the follow-up and the 95.6% with the access to the professionals. Although 18% of subjects would prefer face-to-face visits, most of them (93%) agreed that they would use the telematic procedure again and considered it convenient in the pandemic context. Regarding to the residual events, the median was 3.7 (1.65–6.85). All the clinical symptoms improved significantly after the telematic CPAP treatment (P<.001). Finally, 10 out of the 77 patients included in the study could not be titrated with the telematic procedure.
Comparison of Baseline Data of Both the Hospital (n = 55) and Telematic (n = 55) Groups After PS Matching. Difference in Titration Cost Between the Hospital Clinic Hospital Group (N = 38) and Telematic Group (n = 51).
| Baseline data | Hospital | Telematic | P-Value |
|---|---|---|---|
| Age, mean±SD, years | 55.7±11.5 | 56±11.1 | .900 |
| Male, n (%) | 44 (80) | 41 (75) | .495 |
| AHI, mean±SD, events/hour | 49.2±20.9 | 50.4±19.9 | .747 |
| BMI, median (Q1; Q3), kg/m2 | 31 (27.8; 33.8) | 30.1 (26.3; 34.2) | .432 |
| ESS, mean±SD | 10.2±4.6 | 10.4±5.3 | .863 |
| Titration | |||
| COST (€) | 231.92 | 129.91 | .000 |
| CPAP compliance, median (Q1; Q3), hours/night | 5.8 (4; 6.5) | 6.4 (5.3; 7.1) | .071 |
This new and simple telemedicine strategy proposed in the COVID-19 pandemic is adequate and cost-effective and could contribute to speed up the reduction of waiting lists, with patient satisfaction. We believe that a remote strategy for CPAP titration should be based on (1) the patients should always use their own CPAP, (2) the device should be able to remotely transmit data of CPAP treatment and be able to remote change of parameters which may avoid repetitive appointments for re-titration and (3) a system to hear the patient observations.
FundingSupported by FISPI17/01068.
To Esteve Teijin, Philips Repironics, Cristina Embid and Carmen Leon. Also, the authors want to specially thank the collaboration of Prof. Ramon Farré (University of Barcelona).